Office workers with dry eye symptoms: workplace environment satisfaction and lifestyle effects
Purpose: To investigate the impact of dry eye disease (DED) symptoms and the perception of indoor environmental quality (IEQ) on the well-being and social impact after work in openplan office worker cohort.
Material and Methods: 64 office workers (m= 19; f =45; mean age=47.7±9.3 (sd)), were recruited from a single workplace (local government, open-plan, 400 employees) and asked to complete a DED symptoms questionnaire (OSDI), and answer questions on general ocular health, perception of the IEQ, and social impact from DED symptoms. All participants had worked in the building for at least 4 months.
Material and Methods: 64 office workers (m= 19; f =45; mean age=47.7±9.3 (sd)), were recruited from a single workplace (local government, open-plan, 400 employees) and asked to complete a DED symptoms questionnaire (OSDI), and answer questions on general ocular health, perception of the IEQ, and social impact from DED symptoms. All participants had worked in the building for at least 4 months.
Conclusion: Workers with Moderate-Severe OSDI scores have greater dissatisfaction with workplace environment. A high percentage of workers experienced significant effects on social activities after work.
Introduction
There is increasing awareness of the public health impact of dry eye disease (DED). The personal and economic consequences of DED are thought to be under-estimated.1,2 The impact on quality of life (e.g., decreased work productivity, anxiety) gives DED an influence on the employment, emotional and social aspects of life.3 It is estimated that the economic burden from decreased productivity due to DED exceeds the direct cost of care.2,4,5
Working on a computer causes a decreased blink rate, leading to reduced tear stability and increased tear evaporation. When this occurs in an office environment with low relative humidity (RH) (< 40 %) and/or air draft (> 1.5 m/s), a higher tear evaporation rate can be produced.6,7,8 This desiccating stress leads to a recurring cycle of tear instability, evaporation and surface desiccation,9 and initiates an inflammatory process that produces symptoms, anterior eye surface damage, and decreased tear production. Other ocular pathologies may contribute to reduced tear stability and production, e.g., blepharitis.10
This study investigated the effect of internal environment quality (IEQ) on DED symptoms and social activity after work experienced by workers in a modern, open-plan, office building (with a glass façade facing south) in the Netherlands (built 2003). The building had a history of IEQ issues > 10 years (c. 400 employees) with inconsistent temperature and airflow, and variable direct sunlight due to the glass façade.12 A 2013 renovation created flexible-use workstations, meeting rooms and hall spaces, and special attention was made to the IEQ (e.g., new air control system, placement of plants to improve local RH). Even with these adjustments, the workers continued to report poor DED symptoms. A previous study of office workers in the building (n = 294), reported 30 % with DED symptoms and 5 % diagnosed with DED.
Methods
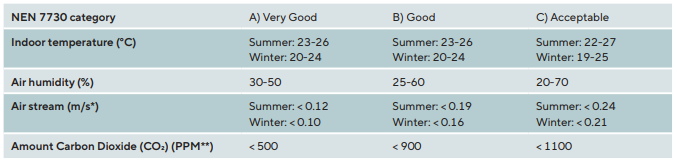
This study was conducted from January – May 2015. During participant recruitment, measurements of indoor air quality were taken every hour (at desk height) at 2 locations on the second floor/south corner of the building, over a 3-week period (26. November 2015 to 15. December 2015): Outdoor air temperature, peak in-building temperature, peak and operative radiation (°C); RH (%), airflow speed (m/s), CO2 level (ppm), draft rate (DR) (%); and light (radiation W/m2). For this study the peak in-building temperature, peak and operative radiation (°C); RH (%), airflow speed (m/s) were most important. In the Netherlands, IEQ quality is regulated by Ergonomics of the Thermal Environment NEN-ISO-7730:2005.11 (Table 1)
All building employees (n = 400) between 18 – 65 years of age were invited to participate. Participants gave consent at a preliminary recruitment visit and were excluded for: pregnancy/breastfeeding, Sjögren’s disease, refractive surgery within the previous 6 months, and working < 4 months in the building. Approved participants were given an appointment for their first visit. All visits took place in the office building, for ease of participant attendance.
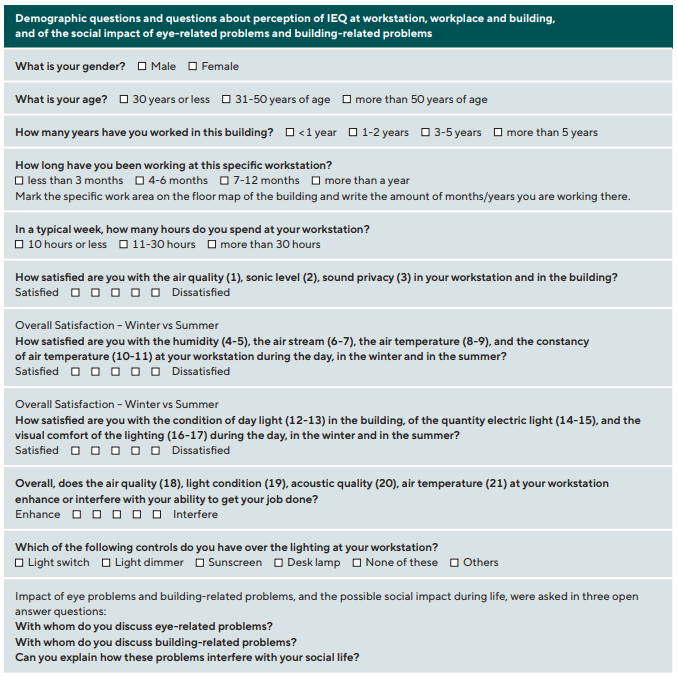
First visit: Visual acuity measured for distance and near with habitual correction. Ocular refraction was determined by auto-refractor measurement. Three questionnaires were given to be completed at home. First: a custom-designed survey on general health, last medical examination, last exam by an eye care professional, any drug prescriptions, allergies and specific vitamin or superfood intake. Second: a custom-designed 21 question, 5-point forced-choice Likert Scale survey on perceived IEQ: satisfaction of light conditions (daylight/electric light), air temperature, workstation RH, and perception of sonic environment during summer and winter; and 4 questions on interference/enhancement of the IEQ (air quality, air temperature, light condition, acoustic quality) on work productivity. The original English version of the Perceived IEQ questionnaire was cultural translated into Dutch and translated back to English. This last English version was used. Third: a custom-designed survey asking about participant IEQ perception and social impact using three open questions: “With whom do you discuss eye-related problems?”, “With whom do you discuss building-related problems?”, “Can you explain how these problems interfere with your social
life?” (Table 2).
Second visit (within 1 month of first visit): The questionnaires were collected, and the participant completed the Ocular Surface Disease Index (OSDI) questionnaire (Research Group at Allergan Inc. (Irvine, California), which surveys DED symptoms during the previous 7 days.
The study was approved by the Human Research Ethics Committee, School of Optometry and Vision Sciences, Cardiff University, and was consistent with the tenets of the Declaration of Helsinki. In the Netherlands, this investigation was considered a routine optometric investigation by the Medical Research Involving Human Subjects Act (2016). All data was filed confidentially and kept anonymous at the point of data entry, with no subjects identifiable.
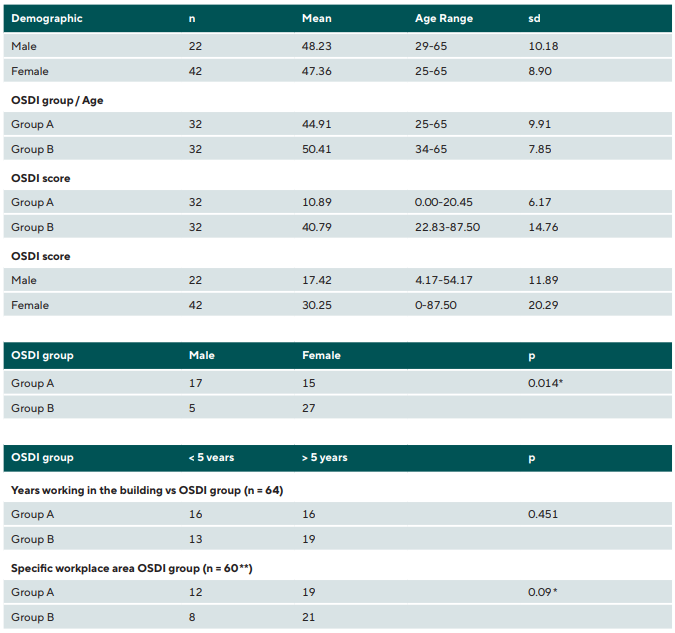
Descriptive statistics were performed on patient demographic data (age, gender, general health and OSDI score) (Table 3). Subjects were grouped according to gender (male/female) and OSDI score (Group A: Normal-Mild score ≤ 22; Group B: Moderate-Severe score ≥ 22.01). Perception of IEQ (satisfaction/dissatisfaction) questions on air quality, RH and light conditions were analysed by gender (male/female) and OSDI group score (A/B). Mann-Whitney U tests assessed differences between males/females. Independent sample tests (t-test) analysed IEQ perception scores between OSDI group. Cronbach’s Alpha coefficient of IEQ questionnaire assessed internal consistency. Logistic regression for gender and OSDI groups were reported as an odds-ratio (OR), with 95 % confidence interval (CI). Questions on working years in the building and time working at the workstation were analysed with Chi-square test.
Results
Sixty-eight employees took part in the study, and 64 participants were included in the analyses (Table 3): 2 participants did not complete the questionnaires and 2 participants chose not to proceed. Most subjects had worked in the building for > 5 years, and > 1 year at a specific workspace (Chi-square: p = 0.013 and p = 0.09, respectively) (Table 3).
There was no difference between genders for questions on ocular and general health, except for males reporting more ocular trauma than females. Females showed a higher predictor for more severe DED symptoms [Odds Ratio (OR): 2.745 (p < 0.001, S.E. 0.299, 95 % CI: 1.533 to 4.948)].
No statistically significant differences were found between OSDI group for number of working hours per day (Mann-Whitney, p = 0.565), per week (p = 0.361), or years working in building (p = 0.451). Significantly more subjects worked > 5 years and > 1 year at a specific workplace in Group 2. No significant difference was found in work experience for gender.
A strong internal consistency was found in perception of occupational IEQ: Cronbach’s Alpha coefficient, 0.923 (coefficient should ideally be > 0.7). No significant difference was found in IEQ satisfaction between males and females, except for degree of satisfaction with workstation air quality (p = 0.016), winter air temperature (p = 0.027), winter temperature constancy (p = 0.018), and quantity of daylight in the winter at workstation (p =0.046), with a greater dissatisfaction by females on these comparisons.
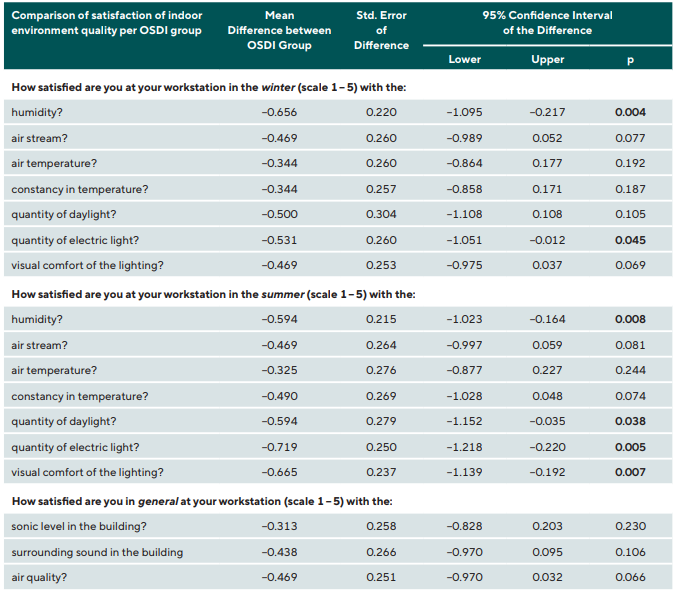
Independent sample t-tests revealed a statistically significant difference between OSDI groups for satisfaction with workplace IEQ, with Group B reporting a more negative score for dissatisfaction with RH in summer (p = 0.008) and winter (p = 0.004), electric light and daylight conditions in summer (p = 0.005 and p = 0.038, respectively), electric light conditions in winter (p = 0.045), and visual comfort of lighting (p = 0.007). All other questions had no significant differences (Table 4).
Testing for IEQ influence on getting work done during the day found no statistically significant difference between Groups A and B for air quality (p = 0.60), temperature (p = 0.741), light (p = 0.540), or sound (p = 0.719).
Sixty-three (98.4 %) subjects reported no control over workspace light switch, 59 (92.2 %) had no control over localised light from a desk lamp, and 34 (53 %) had no control of how sunlight affected their workspace using a sunscreen.
During the 3-week period, the outdoor temperature and the indoor climate were assessed continuously by monitoring the outdoor and indoor air temperature, peak air temperature, operative temperature and relative humidity. According to the NEN-7730:2005 standard, the indoor air temperature just fell within Category C (acceptable) (peak temperature at a sunny day: 24.67 °C), as also did the air flow speed (up to 18 m/s) in the winter, and the CO2 level (up to 900 ppm) (Table 1). The RH showed one dip to 20 % at the peak temperature, but fell within the acceptable range according the NEN standard.
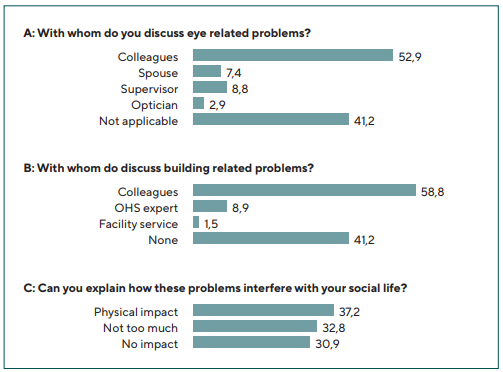
Over 40 % of participants did not discuss their eye-related problems with colleagues or family, nearly 53 % reported discussing with colleagues, nearly 7 % with their spouse, nearly 9 % with their supervisor, and nearly 3 % with their optometrist (Figure 1A). Building-related issues were discussed most often with colleagues (nearly 60 %), with an Occupational Health and Safety (OHS) expert or working consultant (nearly 9 %), and with facility services (nearly 2 %) (Figure 1B).
For social impact, the participants’ answers were categorized into 3 groups based on their answer to the survey question asking how any eye problems affect their social life (Figure 1C): Group 1: No Impact (30.9 % of participants); Group 2: Limited Impact (32.8 %) – complaints were limited and diminished when being at home (getting fresh air, no computer work, or different mindset was enough to ease the burden and not interfere with other daily activities after work); Group 3: Significant Physical and Emotional Impact (37.2 %). Answers reflecting physical and emotional impact were the main factors affecting daily activities: tiredness, headache, not able to watch television or I-pad, not able to drive, or a reason to go to bed early. A small number were unable to wear contact lenses (2 %). More than a third of participants mentioned in general that they needed the weekend to recover from work-related eye problems. Looking at the impact of the OSDI goups vs the social impact the Moderate to severe experience more negative impact after work than the normal-mild group, 62.5 % of the Normal-mild group reported no impact at all, although 70 % of the moderate-severe group reported significant Physical and Emotional impact. Group 2, not too much impact was almost devided in half between the OSDI group A and B (52.4 % for group A and 47.5 % for group B).
Discussion
This study investigated how IEQ was experienced and how IEQ affected well-being and social life. The study found that office workers in this building described dissatisfaction with the IEQ in their building, that dissatisfaction was greater for females and for workers with more severe DED symptoms, and that dissatisfied workers were unlikely to report their dissatisfaction. A previous survey at this location found work productivity and daily activity at work were compromised by eye symptoms experienced at work for a large percentage of workers (n = 193, 74 %).12 The study also found that DED-related symptoms, pain sensation in and around the eye, and light sensitivity, blurry vision, and transient vision were experienced significantly more often at work than at home.
Most participants reported some dissatisfaction in IEQ, with females significantly more dissatisfaction (air quality, temperature, winter temperature constancy) than males. This matches with previously reported gender differences for thermal comfort.13
For difference in IEQ perception between OSDI group, those participants with more severe DED symptoms had greater dissatisfaction with RH in summer (S) (p = 0.008) and winter (W) (p = 0.004), with quantity of electric light and daylight in summer (p = 0.005 and p = 0.038, respectively), and with quantity of electric light in winter (p = 0.045).
Office RH and light conditions are of crucial importance to DED patients. DED office workers are particularly sensitive to the workplace IEQ since DED causes an unstable tear film.15,20,21 Since, the impact of low RH on tear film stability is an important factor in subjective complaints, it is not surprising that subjects with more severe DED symptoms reported a greater dissatisfaction with building RH. The seasonal effects from RH changes are also evident in dissatisfaction with low building RH during winter, and with possible localised lowering of RH caused by ambient temperature increases due to solar radiation.
In the Netherlands, the ISO Standard for Ergonomics of the Thermal Environment (NEN-ISO-7730:2005) is used to predict the general thermal sensation and degree of discomfort for office workers. Thermal sensation is the personal satisfaction with specific aspects of the IEQ, including air temperature, radiant temperature, air velocity, and RH. When office workers complain about indoor IEQ, indoor air measurements are taken. In this study the overall indoor air quality was categorised as ‘good to acceptable’, conforming with the Building Code Guidelines. The RH measurements were low (< 30 %), but within acceptable limits, except for a few sunny days when there was a greater fluctuation in temperature (up to 24.7 °C), RH (down to 18 %), and airflow (up to 0.18 m/s). The consequence of these fluctuations is that IEQ could be acceptable overall, and no intervention is made, while IEQ issues remain. By using the NEN-ISO-7730:2005 guidelines alone, the building classification may not meet the occupational satisfaction of those who work in it who experience eye issues.
In this study, those participants with more DED symptoms reported less satisfaction with the quantity of light they experienced at their workstation. This matches with previous reports of reduced visual-related quality of life score from light sensitivity, and discomfort glare for patients with moderate to severe DED.17,23,24,25 These symptoms can ultimately result in disability glare, and to the more severe, but rare condition of photo-allodynia, caused by a chronic neurotrophic pain.
For participants in this study, their well-being was adversely affected by the building in which they work. This negative illness perception was reported by 60 % of participants who discussed their eye-related problems with colleagues and relatives, compared with 9 % of participants who reported eye-related problems to their supervisor, and only 1 % to the occupational health service. The impact of the IEQ may be seen as a problem that can’t be fixed, or that the supervisor, occupational health care service, working consultant are unable to intervene to change the health problem, or that there is a general lack of awareness in the workers of how these groups can help. There may be evidence for this in the low responses for discussion of any building-related issues with the working consultant (nearly 9 %) or with facility services (nearly 2 %). This negative expectation for a positive intervention could create a negative state of mind in the workers, who may feel that they are not heard or taken seriously.
For the employer, there was some evidence that work productivity is reduced by a negative perception of the work IEQ. Wolkhoff reported that “perceived dry eyes and dry air are associated with deteriorated work performance”.16,19,22 In contrast, the literature suggests that giving employees the ability to adjust their workstation lighting may contribute to better environmental satisfaction and well-being.26,27 In this study, few participants reported the ability to use a sunshield to control the level of sunlight in their workspace. The reflection of sunlight on a computer screen and a lack of technical knowledge in how to adjust the computer screen for changing light conditions during the day could make any discomfort experienced worse. This could be exacerbated by the problem of the south-facing glass façade that may allow fluctuation in light levels (sunlight) throughout the day, leading to discomfort glare. These fluctuations in perceived light were shown by van Duijnhoven et al. (2020), who reported on workstation light conditions in the same building.14
Limitations
The investigation is from a single local Government building in the Netherlands with a known history of complaints about the IEQ. Thus, the participants could be influenced by long-standing complaints and be biased towards a more severely affected symptoms sub-type. However, the even distribution of subjects between the two OSDI score groups suggests that this was not the case and strengthens the statistical analysis. The study location was for a single building, but it can be argued that this location is representative of modern, glass façade buildings with open plan office spaces. The limitation of a single location and small cohort size can be addressed by future studies at other office sites. Other possible causes for DED symptoms were not considered, such as contact-lens induced dry eye or discomfort, effect of blink frequency at the office versus home, or the influence of the specific kind of digital work, or the used software, text size, and contrast.
Practical Implications
It may be possible that building IEQ can lead to work-related DED symptoms caused by increased tear instability and tear evaporation, associated with changes in the blink-rate and RH. This can develop into a negative stress cycle, leading to increased incidence of DED that reduces worker quality of life and productivity. Intervening to prevent this cycle is the first step, and work-related dry eye symptoms should be seen as an occupational hazard in the office environment that must be investigated at an early stage.
Occupational physicians would benefit from being aware of the importance of good tear film stability and visual functioning for the visually demanding tasks of modern office workers.28,29,30 In combination with ergonomics and attention to environmental factors, this will contribute to creating a comfortable working environment. Education about light fluctuations and the ability to adjust the computer screen to avoid reflections and discomfort glare could be an intervention to follow.
There is a need for better education of office workers on the benefits in bringing their concerns to their occupational officer or facility director. Worker awareness about the role of occupational services is needed to get the right help at the right moment, as well as getting good clinical (optometric) diagnostic testing for these symptom
Conclusion
This study helps in understanding the perception and impact of the work environment on eye-related issues. The social impact of work-related eye problems should be investigated further, as IEQ influences are significant and have impact productivity and worker well-being.
Acknowledgments, including all sources of support
Special thanks; Giel Craenmehr, MSc and Ir. M.G.L.C. Loomans, PhD (assistant-professor BPS), Department of the Built Environment, Unit Building Physics and Services (BPS), Eindhoven University of Technology, Eindhoven, The Netherlands.
Conflict of Interests
The authors declares that there is no conflict of interests regarding the methods and devices mentioned in the article.
dry eye disease in the United States: A decision tree analysis. Cornea.
30, 379–387.
Analytical determination and interpretation of thermal comfort using calculation of the PMV and PPD indices and local thermal comfort
criteria”, available at: www.bouwcollege.nl/Pdf/CBZ%20Website/
Publicaties/In%20perspectief/NEN_EN_ISO_7730 (2005 dec).pdf.
Mihucz, V. G., Hänninen, O., de Oliveira Fernandes, E., Silva, G. V. and Carrer, P. (2016). Office characteristics and dry eye complaints in
European workers –The OFFICAIR study. Build. Environ. 102, 54–63.
Harrist, R. and Moore, A. (2009). The effects of an office ergonomics training and chair intervention on worker knowledge, behavior and
musculoskeletal risk. Appl. Ergon. 40, 124–135.
Rooney, T. and Moore, A. (2012). A field intervention examining the impact of an office ergonomics training and a highly adjustable chair on visual symptoms in a public sector organization. Appl. Ergon. 43, 625–631.
