Optometrist: Dry eye management
The integration of modern technology helps in the diagnosis of dry eye. Early detection and treatment prevents progressive tissue loss of the meibomian glands and long-term damage to the ocular surface. Examination of the meibomian glands and evaluation of the individual layers of the tear film should therefore be part of a routine examination by an optometrist. The cause of dry eye is multifactorial.1 Due to changing endogenous and exogenous influences, more and more is being demanded of the tear film's stability. Increasing near activity as well as digital eye strain (DES) contribute to dry eye.2, 3 Studies in different regions show a prevalence of dry eye in children and adolescents ranging from 33% in Colombia4, 15% in the USA5 to 11% in India and 34% of the adult normal population (111 study participants out of 322) fulfilling the TFOS DEWS II diagnostic criteria for dry eye.6 One of the most comprehensive and recent studies in the world clearly demonstrated that the productivity at work and the quality of life of people with dry eye compared to normal eye decrease in proportion to the severity of dry eye.7
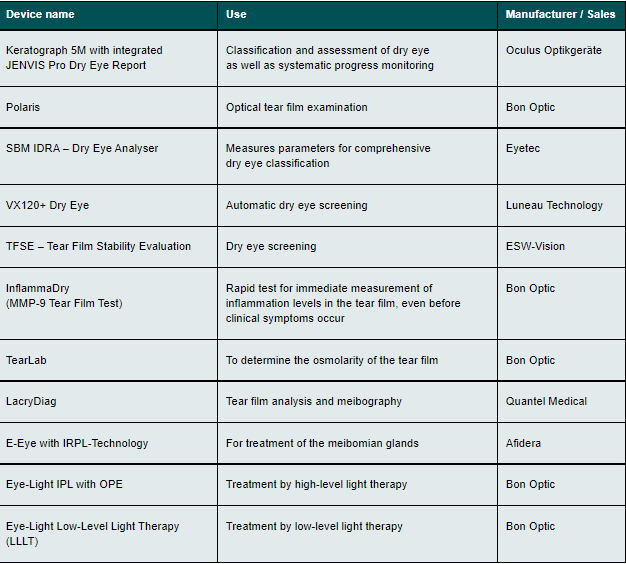
The following devices are used for the diagnosis and treatment of dry eye syndrome*
In addition, there is the causal relationship between eye dryness and the psychological burden.8, 9 It is therefore all the more important to diagnose and treat dry eye as early as possible. Treatment and diagnosis can be done by an optometrist as well as by an ophthalmologist. Especially in the field of contact lens fitting, dry eye and its treatment will play a major role. Contact lens fitters should be trained specifically in this area and be open-minded to modern technologies in order to be able to advise and treat the client in an optimal way, preferably before the physiology of dry eye has progressed and also before the clinical symptoms have become extremely distressing for the patient.Regardless of the choice of examination tool, the optometrist will continue to depend on the patient's reliability and compliance. Success can only be achieved through correct treatment compliance.
The use of software that makes it possible to show the progress of individual therapies enables the patient to participate in the success of the therapy. It is preferable to use a technology which, after the initial examination, determines the same image section of the anterior segment of the eye as well as the ectropionated eyelid, with always the same image marking, for each follow-up examination, in order to be able to establish and document comparability. It is important to differentiate in which form a deficiency exists: is there a secretory tear deficiency (lack of water and mucins) and/or is it a case of hyperevaporation and thus a non-optimal lipid component of the tear.10
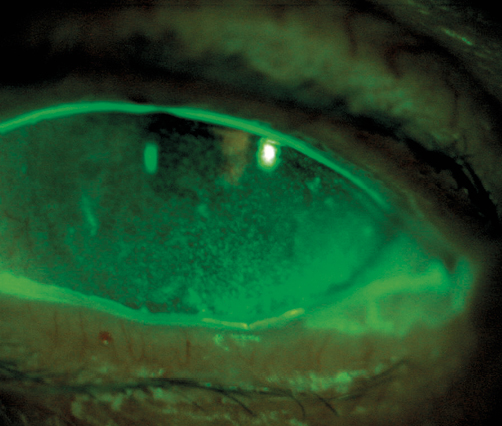
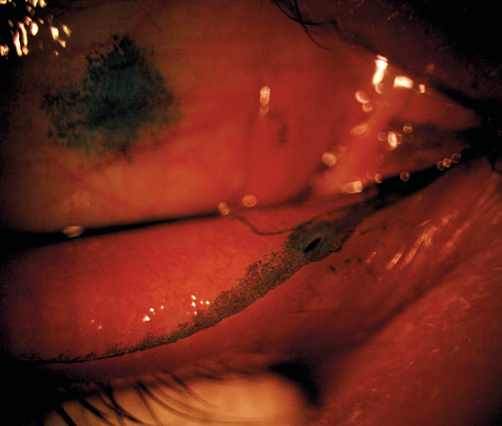
Automatic detection of the meibomian gland dropout also extends the scope to reliably assess the status of therapy and improves the reproducibility of therapeutic success.
There are several therapeutic options for treating patients with dry eyes. Each of them aims to prevent the progression of degenerative processes on the eyelid. Regardless of the method, long-term changes can only be achieved if there is precise instruction by the examiner and good compliance by the patient. A status image of the lipid layer allows partial conclusions to be drawn about the stability of the tear film. If it is intact, the aqueous portion of the tear stays on the eye longer, which increases the tolerance of contact lenses and thus reduces the drop-out rate. If the lipid layer is stabilised by a therapy, discomfort can be reduced and the patient's well-being can be improved. The use of meibography assists in the assessment of meibomian gland dysfunction.
Additional independent studies could clarify whether a slower process in the morphological development of the meibomian glands takes place in older persons through the administration of tear substitutes. Furthermore, the correlation of the morphological change of the glands between the OSDI score and the tear break-up time with the administration of tear substitutes as well as other methods for the treatment of dry eye would remain to be clarified. Furthermore, it would be interesting to find out whether, in addition to the clinical symptoms, the morphological signs are also changed and how long this condition lasts. In this context, subsequent double-blind studies could test the extent to which there are fluctuations with regard to the aforementioned parameters independently of the administration of a tear substitute.
.
Literature References
[1] Department of Ophthalmology and Visual Sciences, The Chinese University of Hong Kong, Shatin, Hong Kong, Chan, T. C., Chow, S. S., Wan, K. H., Yuen, H. K. (2019). Update on the Association between Dry Eye Disease and Meibomian Gland Dysfunction. Hong Kong Med. J.
[2] Sheppard, A. L., Wolffsohn, J. S. (2018). Digital Eye Strain: Prevalence, Measurement and Amelioration. BMJ Open Ophthalmol., 3, e000146.
[3] Blehm, C., Vishnu, S., Khattak, A., Mitra, S., Yee, R. W. (2005). Computer Vision Syndrome: A Review. Surv. Ophthalmol., 50, 253–262.
[4] Rojas-Carabali, W., Uribe-Reina, P., Muñoz-Ortiz, J., Terreros-Dorado, J. P., Ruiz-Botero, M. E., Torres-Arias, N., Reyes-Guanes, J., Rodriguez Zarante, A., Arteaga-Rivera, J. Y., Mosos, C., Gutiérrez, Á. M., Molano-González, N., Marroquín, G., de-la-Torre, A. (2020). High Prevalence of Abnormal Ocular Surface Tests in a Healthy Pediatric Population. Clin. Ophthalmol., Volume 14, 3427–3438.
[5] Tichenor, A. A., Ziemanski, J. F., Ngo, W., Nichols, J. J., Nichols, K. K. (2019). Tear Film and Meibomian Gland Characteristics in Adolescents. Cornea, 38, 1475–1482.
[6] Wang, M. T. M., Muntz, A., Mamidi, B., Wolffsohn, J. S., Craig, J. P. (2021). Modifiable Lifestyle Risk Factors for Dry Eye Disease. Contact Lens Anterior Eye, 44, 101409.
[7] Dana, R., Meunier, J., Markowitz, J. T., Joseph, C., Siffel, C. (2020). Patient-Reported Burden of Dry Eye Disease in the United States: Results of an Online Cross-Sectional Survey. Am. J. Ophthalmol., 216, 7–17.
[8] van Tilborg, M. M., Murphy, P. J., Evans, K. S. (2017). Impact of Dry Eye Symptoms and Daily Activities in a Modern Office. Optom. Vis. Sci., 94, 688–693.
[9] Stapleton, F., Alves, M., Bunya, V. Y., Jalbert, I., Lekhanont, K., Malet, F., Na, K.-S., Schaumberg, D., Uchino, M., Vehof, J.,V iso, E., Vitale, S., Jones, L. (2017). TFOS DEWS II Epidemiology Report. Ocul. Surf., 15, 334–365.
[10] (2017). Kontaktlinsen Know-how, 4. Auflage.; Müller-Treiber, A., Ed.; DOZ: Heidelberg, 2017.