Scleral Shape and Its Correlation With Corneal Topographic Parameters: A Review
Purpose: This review paper aims to summarize the outcomes of the different studies investigating the correlation between corneal and scleral profiles, outline the relationship between corneal and scleral curvatures and asymmetry, and describe the correlation between corneal astigmatism and scleral toricity in regular and irregular corneas.
Material and Methods: Literature was reviewed from PubMed. A total of 48 articles were specifically selected for the current study.
Results: The scleral and corneal radii are directly correlated; the greater the corneal radius, the larger the scleral radius. The cornea and sclera become gradually flatter and asymmetric as the distance from the corneal optical line increases. Similar to the central cornea, the limbal area is more likely to be spherical. The horizontal asymmetry between the nasal and temporal areas is greater than the vertical asymmetry, with the nasal region of the ocular surface being the flattest. In eyes with keratoconus, the sclera is steeper, more asymmetric, and irregular. Cone decentration predicts asymmetric sclera. Corneal and scleral toricity are more likely correlated when corneal astigmatism is greater than 2.00 D.
Conclusion: Some correlations were found between corneal and scleral topography; however, performing both corneal and scleral topography are necessary when fitting contact lenses. Further investigation is needed with larger groups matched in age, refractive error, and biometry and comparing smaller or steepest eyes (i.e., Asiatic population) with larger or flatter eyes. It would also be interesting to compare such correlations in primary and secondary ectasia, investigating whether the scleral shape changes in secondary ectasia.
Introduction
The human anterior ocular surface is rotationally asymmetric.1,2 Generally, the nasal area is flatter than the temporal area,2-7 and the nasal sagittal height is lower than the temporal sagittal height.1,4,8 In addition, the ocular surface exhibits an increase in asymmetry with radial distance from the corneal apex.1,3 However, the corneal and scleral anatomy, and physiology vary with age,9 race,10 time of day,11 refractive error,12 and disease,13 and, consequently, show substantial intrasubject variations.1
Accurate knowledge of the anterior ocular surface is essential when fitting contact lenses. The posterior lens surface needs to align properly with the underlying tissue, providing comfort and maintaining ocular surface health. For soft contact lenses, a mathematical model was developed to evaluate the fit of soft contact lenses on the eye.14 The model considers the interaction between the lens and the ocular surface, considering both the lens‘s geometric properties and the mechanical properties of the eye. Parameters such as tear film thickness and corneal curvature are included in the model. The researchers tested the model using data from soft lens wearers and found that it accurately predicted the fit of the lens in different areas of the eye. They also used the model to simulate how changes in lens diameter and thickness affect the fit. Ultimately, the study suggests that this mathematical model could be a valuable tool for enhancing soft lens design and improving wearer comfort.14 Anterior segment optical coherence tomography (AS-OCT) and scleral topographers provide reliable data on the cornea and sclera, which are helpful in contact lens practice. However, they are restricted to a few clinical practices, and corneal topographers are widely used. Thus, clinicians have greater availability to map the cornea and obtain topographic indices and parameters. Nevertheless, corneal topographic data to predict scleral profiles and aid in contact lens fitting is controversial.
Recently, Bandlitz published a literature review that explores the current knowledge and understanding of the topography (surface characteristics and shape) of the sclera.15 The review covers various studies on scleral topography using different imaging techniques and highlights the importance of accurate scleral topography in the diagnosis and treatment of eye diseases, as well as in the design and fitting of contact lenses.15 This review is different as it focuses on the correlation between corneal and scleral shape. It summarizes the outcomes of the different studies that have investigated the correlation between corneal and scleral profiles, outlines the similarities between corneal and scleral curvatures, describes the correlation between corneal astigmatism and scleral toricity in regular and irregular corneas, discusses whether corneal asymmetry expands into the sclera, and explains the clinical implications of the various outcomes in fitting soft, orthokeratology, and scleral lenses.
Method of research
The literature reviewed was from PubMed using the following keywords, separately and in combination: human scleral shape (508 results), scleral profile (490 results), scleral shape correlation (70 results), scleral topography (298 results), scleral contour (105 results), corneal astigmatism (over 8000 results), scleral asymmetry (79 results), and corneal asymmetry (621 results). From all the articles found, a total of 48 articles were specifically selected for the current study. The selection criteria were articles focused on studies of the corneo-scleral shape in the human eye and the relationship between corneal and scleral shape.
Corneal and scleral radii
Several studies have demonstrated that the sclera is flatter than the cornea.3,5-7,16-20 Although the technology and data analysis methodology applied differed across these studies, the reported results were consistent. A summary of the outcomes is presented in Table 1.
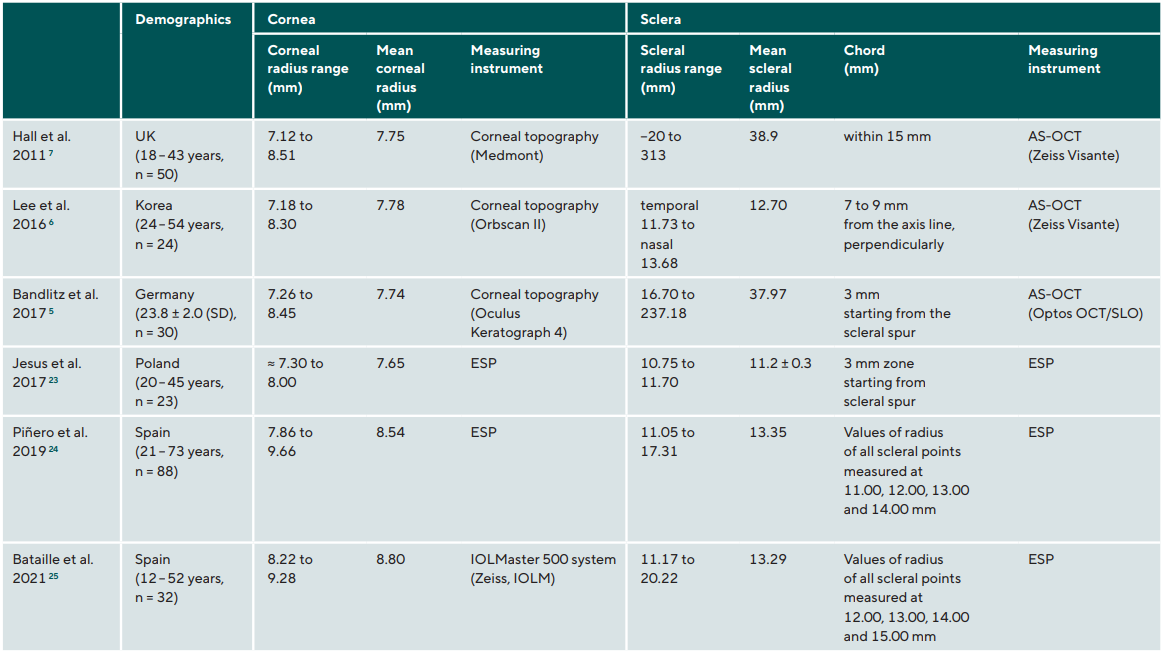
Sorbara et al. measured nasal and temporal tangential angles using built-in AS-OCT software tools as a predictor of scleral shape at 15 mm chord so that they could compare corneal topography to corneal/scleral sagittal height.17 Unlike other studies that described corneal and scleral measurements in radii, they reported scleral measurements in sagittal height and angles. The researchers found a weak, though significant, positive linear correlation between the corneal/scleral sagittal height and the central horizontal corneal radius. However, they found that neither the central radius of the cornea nor the corneal/scleral sagittal height could predict the scleral shape.17 Hall et al. captured the AS-OCT images with the eye in five different gaze directions and then extracted the scleral radius values using the built-in caliper and protractor tools.7 They obtained different values (ranging from –20 to 313 mm) than those reported in later studies, although using the same technology (AS-OCT-Visante, Carl Zeiss Meditec Inc, Dublin, Calif.).3,6 This study showed that it is challenging to measure the scleral radius of curvature manually using a single AS-OCT cross-section image at a time. Choi et al. also used AS-OCT to measure the radius of the anterior scleral curvature; however, their radius calculation approach, while still manual, was more precise.3 They considered the best-fit circle of scleral points from three AS-OCT cross-sectional images assembled manually. However, the authors reported its variance (more than 5 %) and the need for multiple acquisitions as a limitation of their method.3
Subsequently, the same authors used the AS-OCT cross-sectional obtained in a previous study from the same subjects for a more automated analytic method.6 They used ImageJ, a Java-based image processing program that stitches images semi-automatically overlapping them together, with minor adjustments in rotational misalignment. The measurements were performed at five different points of the sclera (from 7.00 to 9.00 mm from the corneal axis line), finding that the scleral radius gradually increases as the distance from the corneal axis line increases. The value of the scleral mean radius observed in the latest study (12.70 mm)6 was very similar to that of previous research (12.82 mm).3 Bandlitz et al. evaluated the ocular surface radii using AS-OCT combined with a confocal scanning laser ophthalmoscope and the ImageJ processing program.5 They also found that the sclera was flatter than the cornea; however, no statistically significant correlation was observed between the central corneal and scleral radii. The scleral radii in this study5 were similar to those reported by Hall et al.7 This may be explained by the fact that in both studies, the tangential scleral radius was assessed, while Choi et al.3 and Lee et al.6 calculated the axial sagittal radius of the sclera using AS-OCT. Tangential and axial radii correspond to different mathematical definitions of curvature and, consequently, cannot be directly compared.
Jesus et al. found a significant correlation between scleral and corneal radii.18 Piñero et al. analyzed the sagittal height for four chords: 11, 12, 13, and 14 mm.19 Corneal and scleral curvatures were calculated as the mean values of the central and peripheral radii of the cornea and sclera, respectively. The peripheral corneal and scleral radii were flatter than the central corneal radii. Since the peripheral cornea is flatter than the central cornea, the entire corneal mean radius was found to be flatter than that previously reported for a healthy cornea when a smaller corneal region was considered.21 The scleral radius was flatter than that found in previous studies.3,6,18 This may be due to the different techniques used (eye surface profiler (ESP, Eaglet Eye, the Netherlands)) compared to that of previous studies (AS-OCT).3,6 Although both Jesus et al.18 and Piñero et al.19 used the same technology (ESP), the calculation approach was different; the first used custom-made software, while the second used ESP software parameters. However, both studies found a significant correlation between corneal and scleral radii; a larger corneal radius corresponds to a greater scleral radius in healthy eyes.18,19 This correlation was stronger in the emmetropic eyes.18 Bataille et al. also used ESP to calculate the scleral radius.20 These values were similar to those of Piñero et al.,19 probably because both studies were conducted in the same location with patients of the same ethnicity.
Summary:
- The sclera is flatter than the cornea.
- In healthy eyes, the greater the corneal radius, the larger the scleral radius.
- The cornea and sclera gradually flatten as the distance from the corneal axis line increases.
Clinical implications:
- A physiologically flat cornea (excluding corneas in post-refractive surgery) will correspond to a flatter sclera.
- Changing the soft lens radius to align to the scleral surface may result in increased squeeze pressure at the lens periphery, which explains the lens fits appearing excessively tight or loose.7
- When fitting an eye with a flat cornea, a flatter scleral lens is needed.
Corneal astigmatism and scleral shape
An earlier study found no correlation between corneal and scleral toricity.22 However, it has been observed that when corneal toricity is congenital, it may expand to the sclera.23 Using the ESP, Piñero et al. measured the ocular surface parameters at chords: 11, 12, 13, and 14 mm.4 In this cohort of participants with corneal astigmatism ranging from −0.20 to −4.60 D, no statistically significant differences were found between corneal astigmatism and scleral nasal-temporal asymmetry.4 In addition, considering healthy eyes with different refractive errors, Niyazmand et al. analyzed the horizontal meridian of ESP maps.24 Their results agree with those of Piñero.4 Measuring healthy eyes but with different technology (AS-OCT), Ritzmann et al. reached the same conclusion;8 however, they found that corneal astigmatism greater than 2.00 D seems to be more likely associated with scleral toricity. These findings are consistent with those of Consejo and Rozema, who investigated scleral shape and its correlations with corneal astigmatism (cylinder ranging from −1.00 D to −3.75 D).25 To avoid the potential bias of other refractive states, moderate or high myopia (< −2.00 D) was considered an exclusion criterion. In this study, no statistically significant difference was found in scleral shape between non-astigmatic and astigmatic participants. However, when isolating the astigmatic component, corneal astigmatism seemed to ‘follow’ scleral toricity. Two main independent parameters were considered when analyzing the corneo-scleral shape: decentration and toricity. A sine function was used to fit the corneoscleral profile, with the first term (decentration) representing eye position with tilt and making the biggest contribution, the second term (toricity) representing astigmatism, and the remaining terms representing smaller, more irregular contributions that could be disregarded. When considering corneoscleral profile components independently, no statistically significant differences were found between astigmatic and non-astigmatic eyes in decentration, but statistically significant differences were found (p << 0.001) when comparing toricity on its own between groups. Therefore, when analyzing scleral shape as a whole, without separating it into its contributing components (decentration, toricity, and other minor contributions), no statistically significant difference was observed between non-astigmatic and astigmatic participants, in agreement with other works.4,8,24
Macedo-de-Araújo et al. compared corneal topography data with scleral lens parameters.26 The authors found that in subjects with limbus-to-limbus corneal astigmatism higher than 2.00 D, the sclera exhibited a toric shape with the same orientation. Although in this study26 the scleral profile was deduced indirectly by assessing scleral lens behavior in the eye, the outcomes were similar to those of previous reports.8,25 There was a positive correlation between corneal and scleral shape when corneal astigmatism is greater than 2.00 D. López-Álcon et al. also investigated the relationship between corneal and scleral toricity orientation by measuring scleral toricity indirectly through the stabilization of toric scleral lenses.27 In only 27 % of cases, there was a similarity between the values with a maximum error of 10°. The low correlation shown in this study may be due to the fact that 60 % of eyes had astigmatism lower than 2.00 D.
Summary:
- Corneal astigmatism greater than 2.00 D tends to be correlated with scleral toricity with the same orientation.
Clinical implications:
- Corneal topography may predict the presence of scleral toricity when the corneal astigmatism is greater than 2.00 D.
- Eyes with high corneal astigmatism may more likely need a toric scleral lens.
Corneal and scleral asymmetry
Corneal asymmetry
Studies investigating orthokeratology lens decentration and pre-treatment corneal topographic parameters have shown that the cornea is characterized by a significant asymmetry between quadrants.2,28,29 Maseedupally et al. found that the difference in corneal curvature at chord 5 mm was relatively low between the four corneal quadrants (0.22 D between the opposite quadrants) and tended to significantly increase between the chords of 5.00 to 8.00 mm, with the mean temporal-nasal difference being 1.66 D, and the inferior-superior difference being 0.70 D.2 The authors also reported differences in asymmetry between the central and peripheral corneas. In the central cornea, the nasal area was the flattest, followed by the temporal, superior, and inferior quadrants. In the peripheral cornea, the nasal quadrant was still flatter; however, it was followed by superior, inferior, and temporal areas. Chen et al. found similar results with the inferotemporal quadrant of the cornea at 8.00 mm chord to be the steepest region.28 According to the authors, this paracentral corneal asymmetry explains the inferotemporal decentration of orthokeratology lenses that generally have an alignment curve between the chords of 7.00 to 9.00 mm approximately.28 Similar findings were observed in the study conducted by Gu et al.29 The central cornea showed non-significant asymmetry between opposite quadrants and tended to increase towards the paracentral area gradually. This study also revealed that corneal asymmetry was greater in the quadrants of the horizontal meridians.29
Ritzmann et al. investigated anterior ocular surface shape using AS-OCT.8 In contrast to previous reports that measured corneal radii,2,28,29 they assessed the sagittal height of the cornea at a 10.00 mm chord in the eight primary meridians. The AS-OCT measurements showed a significant difference in sagittal height between the region with the greatest height and the least (right eyes 91 μm, left eyes 98 μm). The greatest sagittal height difference between the opposing quadrants was slightly higher in the left eye.
Scleral asymmetry
Several studies aimed to analyze scleral profiles to assess scleral radius3,5-7,19,30,31 or scleral elevation height.1,8,19,32 All
studies found that the sclera presented a significant asymmetry between quadrants despite the different instrumentation and calculation approaches used. The nasal sclera was significantly flatter than the temporal sclera.
Indeed, most scleras exhibit an asymmetrical shape. DeNaeyer et al. analyzed the scleral profile of 140 scleral lens patients using sMap3D (Precision Ocular Metrology, Mexico, USA, distributed by Visionary Optics, Virginia). They found that 66.7 % of the eyes exhibited asymmetrical scleral contour.33
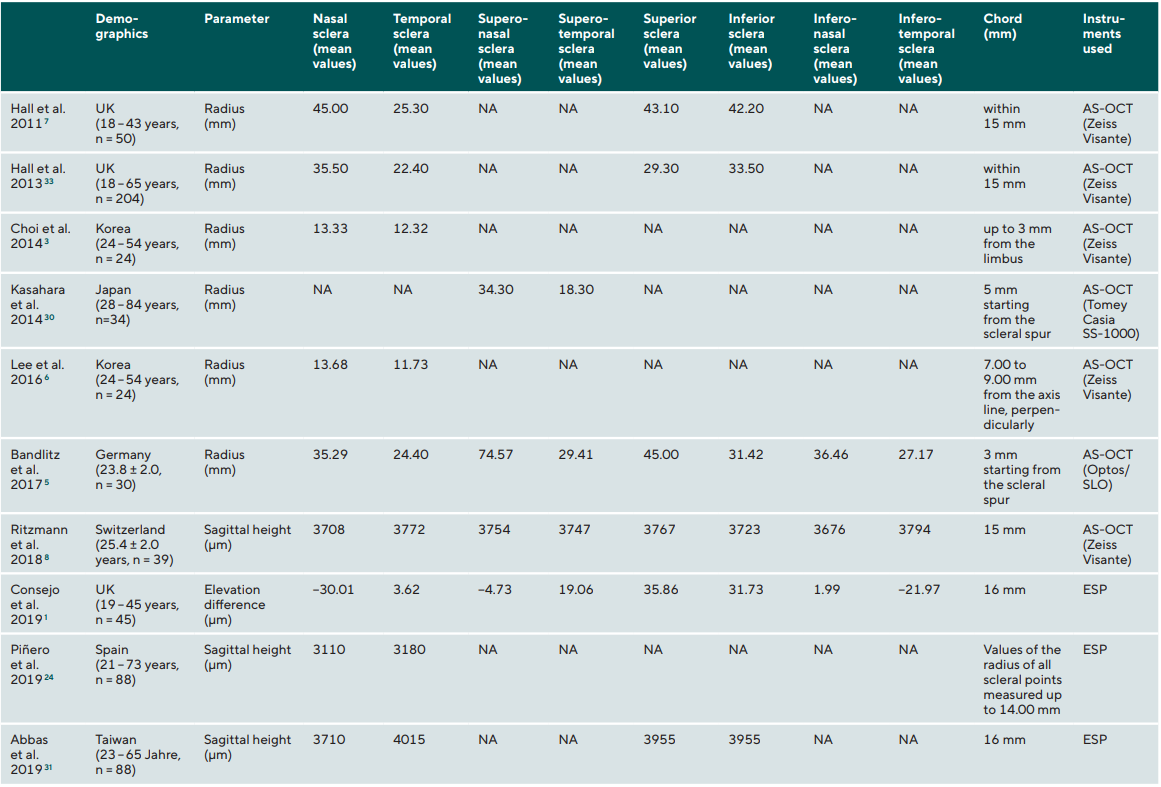
Using an AS-OCT, the measurements of scleral radii differed between studies.3,5-7,31 However, all showed similar conclusions regarding asymmetry: the temporal area was the steepest, and the nasal region was the flattest. Hall et al. found that the mean scleral radius was steepest in the temporal area and flattest in the nasal portion but similar in the other vertical quadrants.7 In a different study, Hall et al. found that the temporal sclera is the steepest, followed by the inferior and nasal areas.7 Choi et al. found that the scleral radius was significantly greater in the nasal sclera (13.33 ± 1.12 mm) than in the temporal sclera (12.32 ± 0.77 mm).3 The same authors, in a successive study found similar values (temporal area 11.73 ± 0.61 mm, nasal area 13.68 ± 0.71 mm).6 Kasahara et al. also showed that the sclera was significantly steeper in the temporal area.31 A later study by Bandlitz et al. found that the scleral flatter region was the superonasal region, followed by the superior and the steepest areas, followed by the inferotemporal region.5 Hall et al.7,34 and Bandlitz et al.5 reported tangential scleral radius, while Choi et al.3 and Lee et al.6 calculated the axial scleral radius. Thus the values can not be directly compared.
Using an AS-OCT, Ritzmann et al. measured the ocular sagittal height at two chords: 12.80 and 15.00 mm.8 At chord 12.80 mm, the sclera appeared more likely to be symmetrical with a non-significant difference between the regions. The measurements at chord 15.00 mm, showed a more rotationally asymmetrical sclera. The difference between the areas with the greatest and least sagittal heights was greater in the right eye than in the left eye. The sagittal height difference between the opposite quadrants was the greatest between the superotemporal and inferonasal quadrants in the right eyes and between the nasal and temporal areas in the left eye.8 These outcomes confirm that the ocular surface becomes more asymmetrical toward the periphery. The nasal scleral area was flatter than the temporal area, and the asymmetry was most significant between the horizontal quadrants.
Consejo et al.,1 Piñero et al.,19 and Abbas et al.32 used an ESP to analyze the scleral shape. Consejo et al. found that the sclera is rotationally asymmetric. The nasal area showed significantly less elevation than the temporal area, and the inferior area was slightly less elevated but not statistically significant compared to the superior area.1 The difference in scleral elevation was found to be greater in the horizontal meridian, which agrees with the findings of previous studies.5,7,8,34 This study also confirms that the sclera becomes more asymmetrical with radial distance, and the difference in elevation between quadrants tends to increase.1 These outcomes coincide with those reported by Piñero et al.19 The asymmetry increased with the diameter of analysis, accounted as an increasing difference between the minimum sagittal height and maximum sagittal height, which grew progressively. The mean elevation difference between the nasal and temporal areas also increased progressively toward the periphery.19 Abbas et al., although using different calculation approaches, showed similar findings: scleral asymmetry was significant between the nasal-temporal quadrants and non-statistically significant in the superior-inferior direction, and the nasal sclera is flatter than the temporal.32
Correlation between corneal and sclera asymmetry
Both corneal and scleral shapes present a significant asymmetry, which is the lowest in the center and gradually increases toward the periphery (Table 2). The central cornea, within 5.00 mm, exhibits a rotationally symmetrical shape. The asymmetry starts at 5.00 mm at increases toward the corneal periphery. In the limbal area, from chord 12.00 19 to 12.80 mm,8 the ocular surface exhibits a rotationally symmetrical profile. The scleral asymmetry becomes significant beyond such chords and increases progressively toward the scleral periphery. The anatomy of the extraocular muscles is believed to be responsible for increasing scleral asymmetry toward the equator.35,36 Additionally, the asymmetry between opposite quadrants, for both the cornea and sclera, is greater in the horizontal meridian, and the ocular surface nasal area is flatter than the temporal area.
Summary:
- The central cornea exhibits a rotationally symmetric shape.
- Around the limbus, the ocular surface is more likely rotationally symmetric.
- Two-third of scleras exhibit an asymmetrical profile.
- The peripheral cornea, similar to the sclera, presents significant asymmetry between quadrants.
- The horizontal asymmetry of the ocular surface is greater than the vertical asymmetry.
- The ocular surface nasal area is flatter than the temporal area.
- The ocular surface asymmetry tends to increase gradually towards the periphery.
Clinical implications:
- Corneo-scleral measurements allow better prediction than central keratometry and videokeratoscopy data of lens fit.
- Soft,7,37 ortho-k,2,28,38 and scleral lenses39 tend to exhibit inferotemporal decentration.
- Any lens decentration may induce astigmatism, affecting visual outcomes,40 especially in multifocal contact lenses.41,42
- Ortho-k lens decentration displaces the treatment zone, leading to poor visual outcomes due to induced astigmatism, increased comatic high-order aberrations (HOAs), and glare.43
- Elevated HOAs induced by ortho-k treatment (mostly spherical aberration and horizontal or vertical coma) have been associated with slower axial eye growth in myopic children.44,45
- Scleral lens decentration displaces lens optic inducing astigmatism, prismatic effect, and vertical and horizontal coma, not corrected by the post-lens fluid reservoir. This adversely affects visual performance.39,46
- Quadrant-specific designs or customized lenses are indicated when better lens centration is required.
- Quadrant-specific designs and customized scleral lenses are indicated for better lens centration since most eyes exhibit an asymmetrical sclera.
Correlation in patients with keratoconus
As soon as researchers started gaining knowledge on the shape of the corneo-scleral profile in the healthy eye, efforts were made to investigate whether the results reported in previous sections were transferrable to compromised eyes. In particular, there is an increasing interest in accurately characterizing the anterior corneo-scleral profile of keratoconus patients because they often benefit from scleral lens wear to improve their vision and, consequently, their well-being.
Using corneo-scleral topography, Piñero et al. provided evidence that the corneoscleral profile in keratoconus presents higher asymmetry than in healthy eyes, especially in eyes with moderate and advanced stages of the disease.47 They also observed that when the cornea steepens in keratoconus, the sclera also tends to steepen. These results are in agreement with those from DeNaeyer et al.,48 who found a statistically significant difference in intra-meridional differences in sagittal height between participants with corneal ectasia and controls. They also found a strong correlation between scleral asymmetry and the level of decentration of the corneal cone,48 suggesting that cone decentration plays a role as a predictor of scleral asymmetry in advanced cases of ectasia. This was further investigated by Dhaese et al., who found a moderate correlation between scleral toricity and the level of cone decentration.49 The latter study included early and mild keratoconus patients, and consequently, with a smaller cone decentration level than that of participants from DeNaeyer’s study,48 suggesting that disease severity may play a role in the influence of cone decentration as a potential predictor of scleral toricity. Using height data, Dhaese et al. demonstrated that with corneal steepening, the sclera tends to steepen in the same semi-meridian, but this was not the case for corneal flattening.49 In other words, the sclera tends to ‘follow’ the steepest angle of the cornea, but there is no clear evidence that this is the case for the flattest angle. Moreover, the relative angle between the steepest and flattest regions in the sclera is highly patient-dependent, hampering the prediction of the optimal toric lens solely from corneal data. In addition, when analyzing keratometry values measured with Pentacam HR, they found that keratometry readings (flattest, steepest, and maximal keratometry) are positively correlated with the level of scleral toricity. Namely, the more irregular the cornea (larger difference between keratometry (K) readings), the more irregular the sclera will be.49 As for corneal astigmatism, measured with a corneal topographer, no correlation was found between scleral toricity and irregularity in eyes with keratoconus.26,49
To investigate the influence of regular contact lens wear on the corneoscleral shape, Van Nuffel et al.50 studied three groups of severity-matched keratoconus patients (group A: lens-naive group; group B: patients regularly wearing corneal lenses; and group C: scleral lens wearers) and compared them with a group of control emmetropic subjects. Their results showed that both corneal and scleral lens wear resulted in significant regional changes in the shape of the corneal periphery and sclera. The peripheral cornea and sclera were found to be significantly steeper in eyes with keratoconus. Additionally, within the keratoconus groups, the researchers reported the highest values of scleral asymmetry in the scleral-lens-wear group. The findings of high scleral asymmetry in keratoconus eyes suggest that scleral lenses with a spherical landing zone will likely result in uneven compression across sectors.
Summary:
- In eyes with keratoconus, the corneoscleral profile exhibits a high level of asymmetry.
- With the advancement of keratoconus, the sclera becomes steeper.
- The sclera may exhibit more irregularity when the ocular surface steepens.
- The peripheral cornea and sclera are significantly steeper in keratoconus.
- In keratoconus, the corneal profile can help predict the presence of scleral asymmetry or irregularity and indicate the location of the steepest scleral angle (semi-meridian).
- In moderate to advanced keratoconus, cone decentration may be considered as a detector of scleral asymmetry.
Clinical implications:
- Cone decentration may indicate the need for a scleral lens with a quadrant-specific design.
- When fitting scleral lenses in advanced keratoconus:
- In some cases, the lenses may benefit from the use of quadrant-specific or customized landing zones.
- Lens periphery may be steeper than usual.
Discussion and conclusion
Correlations were found for different parameters when comparing corneal and scleral topography. The sclera is flatter than the cornea, and the radii of both structures are positively correlated; the greater the corneal radius, the larger the scleral radius. The cornea and sclera become gradually flatter and asymmetric as the distance from the corneal axis line increases. Similar to the central cornea, the limbal area is more likely to be spherical. The horizontal asymmetry between the nasal and temporal areas is greater than the vertical asymmetry, with the nasal region of the ocular surface being the flattest. In eyes with keratoconus, the sclera is steeper, more asymmetric, and irregular. Cone decentration predicts asymmetric sclera. Regarding the relationship between corneal and scleral toricity, it has been shown that they are more likely to be correlated when corneal astigmatism is greater than 2.00 D.
Although corneo-scleral technology provides more information on the ocular surface shape and helps optimize lens fitting, both corneal and scleral topography may be beneficial when fitting contact lenses. A flat cornea indicates a flat sclera; thus, a flat lens periphery is needed, while in eyes with keratoconus, a steeper scleral lens periphery is required. Corneal astigmatism greater than 2.00 D predicts the necessity of a scleral lens with a toric periphery. Additionally, quadrant-specific designs or customized peripheries are indicated when fitting scleral lenses because most eyes exhibit a significant scleral asymmetry, especially in eyes with keratoconus.
Further investigation is needed with larger groups matched in age, refractive error, and biometry since these are known to affect the corneo-scleral shape. This is especially relevant in studies on keratoconus and other corneal pathologies. In the case of keratoconus, it is of paramount importance to evaluate the influence of cone decentration and other corneal parameters considering eyes matched for disease severity. In other words, the impact of the disease stage on the corneoscleral profile is yet to be defined. Additional research is required regarding the correlation between corneal and scleral parameters comparing smaller or steepest eyes (i.e., Asiatic population) with larger or flatter eyes. It would also be interesting to compare such correlations in primary and secondary ectasia, investigating whether the scleral shape changes in secondary ectasia.
Copyright by Daddi Fadel
