Binasal Occlusion for Partly Accommodative Esotropia
Purpose: Utilization of binasal occlusion in the treatment of partly accommodative esotropia and abnormal sensory fusion in a toddler is described.
Material and Methods: Binasal occlusion in the form of translucent adhesive tape was applied to the child’s glasses such that its temporal border bisected the pupil of each eye.
Results: Partly accommodative esotropia with abnormal sensory fusion improved to esophoria with good sensory fusion.
Conclusion: Binasal occlusion is an effective tool in a young patient with partly accommodative esotropia.
Introduction
Esotropia early in life has several etiologies including uncorrected hyperopia. A more precise term may be “association” as only some hyperopic children develop esotropia.1 There are two types of esotropia associated with hyperopia 2 which are distinguishable when refraction and subsequent treatment, prescription eyeglasses for hyperopia, is implemented. Refractive accommodative esotropia leads to a non-strabismic eye posture with glasses in place. The second type, partly accommodative esotropia, is the diagnosis when the glasses incompletely reduce the magnitude of the esotropia.
It has been proposed that partly accommodative esotropia could potentially be a result of delay in treatment.3 The hypothetical etiology for this suboptimal outcome is rooted in the eyeglass delay and depicted in Figure 1. While unaided and esotropic for months or years, sensory maladaptations of suppression and/or anomalous correspondence (AC) arise and become embedded. When glasses are ultimately prescribed, sensory maladaptations override part or all of the divergence motor signal of the plus lenses and esotropia remains. Potential antecedents leading to delay are depicted in Figure 1. Strengthening the likelihood of pathway A, cosmetically non-obvious small angle esotropia at onset, is that small angle esotropia is associated with a greater propensity for anomalous correspondence.2 Additionally, small strabismus angles often go undetected delaying treatment.
This delay-in-treatment etiology is speculative. An Occam’s Razor explanation is that the esotropia was never destined to be anything but a partly accommodative esotropia plausibly because of a low AC/A ratio.2 The magnitude of the hyperopia/esotropia and the antecedents to diagnosis and treatment have no bearing on the ultimate diagnosis. Additionally, it has been proposed that a delay in eyeglasses for hyperopia may cause deleterious changes to the medial recti muscle so that a nonaccommodative eso deviation develops.2 In this interpretation, muscle alterations, not sensory maladaptations are the principle cause. Support for embedded sensory fusion anomalies due to eyeglass delay causing unfulfilled refractive accommodative esotropia can be found if abatement of the sensory maladaptations is attempted. Abatement of the sensory fusion abnormalities, particularly anomalous correspondence (AC), may convert partly accommodative esotropia to refractive accommodative esotropia. This case report demonstrates exactly this outcome. Partly accommodative esotropia converted to fully accommodative esotropia after a sensory fusion normalizing treatment method, binasal occlusion,4 was employed.
Case Report
Case History
“CJ”, 31 months old female, presented with her parents who were seeking a second opinion for treatment of their daughter’s esotropia that was not surgical. Their daughter’s eyecare began when parents noticed crossing eyes when she was 16 months old. The crossing began as a variable inconsistent inward misalignment that worsened slowly. As shown in Table 1, her first eye exam at age 17 months resulted in a diagnosis of constant alternating esotropia magnitude 25^BO coupled with high hyperopia. Eyeglasses (+6.50 DS / +7.00 DS) were prescribed for full time wear. Due to a complex set of circumstances, including a frame that fit poorly and prohibited regular wear, daily full-time wear of eyeglasses did not commence until she was age 20 months – 4 months after onset of the esotropia. CJ readily accepted the eyeglasses and wore full time as instructed. With glasses in place, the crossing eye concern was mitigated per parent observation. A follow up exam with her eye doctor, age 20 months in Table 1, confirmed resolved esotropia with glasses in place. Accommodative esotropia was diagnosed. Parental observation and follow up evaluations revealed recurrence of esotropia while corrected (age 26 and 29 months in Table 1). The parents estimated that the recurrence of the inward crossing began approximately 3-4 weeks after wearing glasses full time. Parents had some uncertainty but assigned the crossing to the left eye.
The parents were apprehensive about a recent recommendation from their daughter’s eye doctor that eye muscle surgery was the next step in treatment of CJ’s esotropia. They wanted to know if there were alternative treatments. The eye crossing was described as present with glasses on and increasing in magnitude and frequency over the past few months. Glasses off, the crossing was marked.
CJ has hearing impairment for which she wears hearing aids. Otherwise, she is generally a healthy, vibrant, cognitively advanced toddler. She was born at a normal weight after a full-term pregnancy to a healthy non-smoking mother. Developmental milestones are on time with language, especially receptive language, rated as advanced. CJ is learning sign language at a rapid clip. Family history is unremarkable and non-contributory. At all exams she appeared healthy and well-nourished with above age typical testability. She is sociable, has good eye contact, and good understanding of non-verbal cues.
Evaluation 1
The author’s first exam of CJ, age 31 months, resulted in a diagnosis of very high frequency alternating esotropia magnitude 25^BO with glasses in place. OD was the preferred eye for fixating. It is important to point out here that the 25^BO matches the magnitude of the unaided esotropia at her first eye exam with her original eye doctor (age 17 months in Table 1). The eso deviation was concomitant per monitoring Hirschberg corneal reflections during versions. Ductions were full each eye in the abduction direction. The glasses (+6.50 DS OU) afforded 20/25 VA each eye using Cardiff Cards two-item forced choice modality.5 Monocular estimate method (MEM) Near retinoscopy 6 with glasses in place revealed +1.00 lag each eye. Distance retinoscopy over her glasses resulted in plano DS each eye.
Sensory fusion testing using the 3 Figure Flashlight 6 while CJ wore red green goggles over her spectacles resulted in a reliable response of seeing 3 shapes. Evincing precociousness, CJ counted the shapes and named them (ball, girl, elephant) correctly in a few seconds. It could not be determined if she was aligned or esotropic during this response because of poor visibility of her eyes behind the red/green goggles and the brevity of her interest in viewing the second degree fusion targets. If esotropic, the likely circumstance, this response equates to anomalous correspondence. If aligned the interpretation is normal second-degree fusion. Additional sensory fusion testing with Lang Stereo 7 and Frisby Stereo 7 led to equivocal responses that could not be equated with seeing floating targets.
Deteriorated accommodative esotropia with probable anomalous correspondence was diagnosed. The suspect anomalous correspondence diagnosis is based on her response to the 3 Figure Flashlight and conversion from aligned with glasses in place to esotropia while corrected. Binasal occlusion (BNO) was prescribed. Parents were educated that it would be optimal for CJ to have two pairs of eyeglasses so that binasal occlusion could be applied to one of the two eyewear to facilitate a wearing schedule. The eyeglass prescription was not changed.
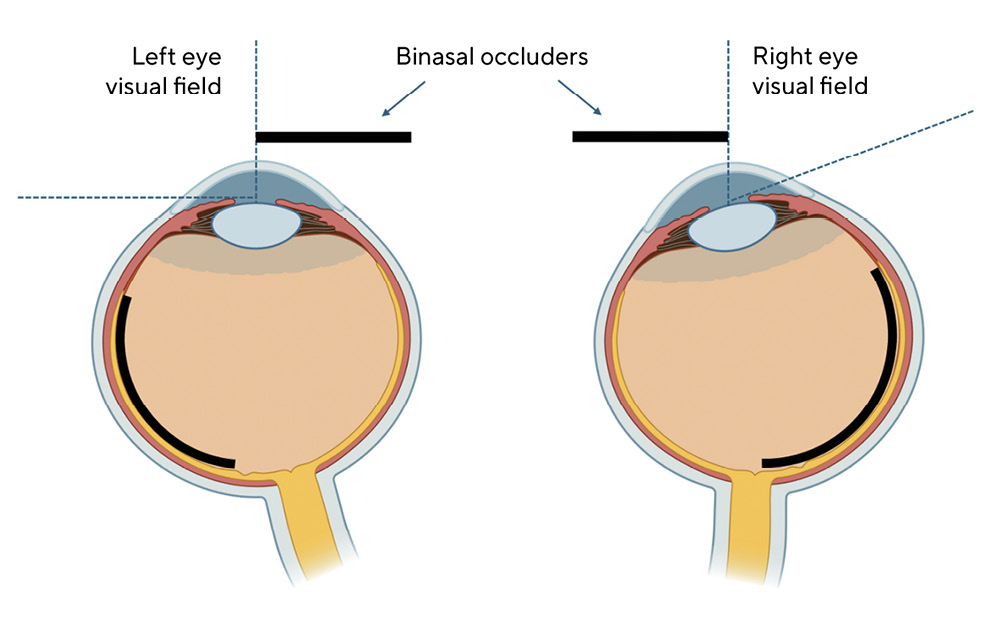
The parents returned three weeks later with the recommended two eyeglasses. Binasal occlusion was applied to one of them following the method described by Greenwald for alternating esotropia.4 In brief, the pupils are bisected by ordinary translucent adhesive tape applied to the ocular side, nasal portion, of the eyeglass lenses. The tape spans the ‘B’ dimension of the eyeglass lens as shown in Figure 2. Immediately after application CJ did not demonstrate resistance or distress. Parents were instructed to have CJ wear these glasses full time unless she demonstrated high resistance. If resistant, a realistic possibility with binasal occlusion, set a goal of as much as possible. Another instruction should resistance occur was to start with one hour per day and increase an hour per day. A follow up evaluation was planned for six weeks. CJ’s home environment was rich with developmental activities, including motor and visual motor, so that additional home developmental visual activities were not specifically assigned.

Evaluation 2
CJ, aged 34 months at this evaluation, presented wearing the glasses with BNO. Mother reported that CJ had been wearing the BNO glasses full time since application with no signs of aversion or changes in her activities of daily living. She stated that visible crossing was less often and of lower magnitude. Unilateral cover testing showed low frequency intermittent alternating esotropia. Alternate cover testing revealed a magnitude of 10^BO at far, 14^BO at near. Frequency of the esotropia was estimated to be 20 % based on the 15 – 20 seconds of cover testing CJ permitted. Monocular and binocular visual acuity with glasses in place remained good with Cardiff Cards. Stereopsis was 215 seconds per Frisby. All three shapes were seen on the 3 Figure Flashlight and a unilateral cover test confirmed no tropia during this response. To see the unilateral cover test result, lighting was high and an examiner strategically positioned close to CJ to see through the red green goggles. Near accommodation was accurate, +0.50 lag, per MEM retinoscopy. Accommodative esotropia with residual esophoria in a convergence excess pattern was diagnosed. Sensory fusion is normal. Parents were instructed to cycle in the ordinary eyeglasses (no BNO) one or two hours per day
Evaluations 3 & 4
Three months then seven months later CJ was evaluated with the same favorable results. She remained esophoric with good sensory fusion per Frisby stereo test and pediatric flashlight. At each evaluation visual acuity was 20/25 monocular using Lea single optotype without crowding.8 Following evaluation three, BNO was reduced to 4 days on / 3 days off. Evaluation four concluded with a reduction to 2 days per week. A six-month follow-up was recommended which did not take place at the time of this draft.
Discussion
BNO with ordinary frosted household translucent tape attenuates light and prohibits form from striking the geographic temporal retinae. For an eye in primary gaze geographic and anatomical temporal retina coincide. In an esotropic adducted eye, the fovea and a portion of nasal retina are in the geographic temporal retina as shown in Figure 3. While a large swath of the retina is occluded in an esotropic eye, occlusion of the fovea is the hypothetical key for the efficacy of BNO as described by Petito et al and in the next paragraph.9
For patients with esotropia, under normal viewing conditions the fovea of the esotropic eye receives an image that is temporal to and different from the target of regard on the fovea of the fixating eye. If sensory fusion is normal, this mismatch gives rise to visual confusion; a perception of different items overlapping and occupying the same spatial location.10 To resolve this untenable visual percept, brain suppresses the fovea of esotropic eye and may suppress nasal retina or rewire its cortical representation to anomalously correspond to the fixating eye. If this maladaptation embeds, treatments intended to restore bifoveal fixation (eye muscle surgery, prism, or convex lenses for hyperopia) may be overridden to maintain the abnormal sensory fusion status quo. The mechanism for this override, anomalous fusional convergence, results in re-establishment of esotropia. In CJ’s case, this can be seen the resumption of a 25^BO esotropia at near with glasses (31 months in Table 1) which mirrors the 25^BO baseline esotropia present while unaided (17 months in Table 1). A plausible explanation is that she activated anomalous fusional convergence to resume the motor alignment posture in which the esotropic eye has a nasal retinal areal aligned with the fovea of the fixating eye.
BNO, by occluding the fovea of the esotropic eye, relieves the brain of visual confusion arising from mismatched foveal images. In response, brain relaxes its suppression and anomalous correspondence strategies and turns on normal sensory fusion that was utilized prior to the onset of the esotropia. If a motor signal for alignment such as convex lenses for hyperopia is present it may now take place free of the counteracting impetus of anomalous fusional convergence.
This case clearly had all the elements of refractive accommodative esotropia. At onset the inward crossing was variable and her age, 16 months, is characteristic.2 Her hyperopia was very high and its uncorrected magnitude, 25^BO, at least on paper, should result in ongoing consistent bifoveal alignment if optimal hyperopic correction is worn. There were logistical delays in obtaining the glasses such that she functioned as a constant esotrope for 3-4 months. Thanks to good clinical records and parents who were good observers and historians, a reliable conclusion is that the glasses yielded alignment for a short time via AC/A. Esotropia recurred after 3-4 weeks because of anomalous fusional convergence which is known to be slow.11 BNO turned off anomalous correspondence and the AC/A driven divergence from the convex lenses for her hyperopia decreased the eso magnitude sufficiently for bifoveal alignment to manifest.
One inconsistency in this case and the BNO theory offered is CJ’s notable residual esophoria. After sensory fusion was normalized, why didn’t the full hyperopic correction convert the magnitude 25-30^BO unaided esotropia to orthophoria status she enjoined at her age 20 months evaluation? (Table 1) It makes the case that she had two forms eso deviation. One, approximately 20^BO, due to uncorrected hyperopia. The other was an additional non-accommodative esophoria, approximately 10^BO. This progressive increase in eso over time among individuals with accommodative esotropia has been described in the literature.2 Specifically, the literature describes deterioration into esotropia with the glasses on from a previously aligned state.2 Without BNO, CJ’s residual esophoria could very well have remained as esotropia and CJ would be classified as just another child with partly accommodative esotropia.
Because complete monocular occlusion turns off abnormal sensory fusion 12 it could be argued that monocular occlusion could normalize alignment in the same manner as BNO. BNO, however, arranges conditions so that the esotropic eye is receiving some visual input as opposed to zero in full occlusion. The visual input strikes nasal retina as shown in Figure 3. If occlusion of the fovea brings previously operational normal sensory fusion online, the nasal retina is not suppressed and normal correspondence is activated. This disparity with the fellow eye will result in uncrossed diplopia and may prompt fusional divergence to resolve the diplopia. Repeated activation of fusional divergence enhances it so that confronted with a moderate to high esophoria upon cessation of BNO later, as was CJ, it can be overcome with ease.
Two final comments on this case and BNO in general have to do with acceptance of the treatment by the patient and its success in this case. CJ’s ready acceptance of BNO was remarkable. When it was applied for the first time in the clinic optical dispensary, her interest in the busy environment heightened. As instructed, mom was holding her hands to prevent immediate removal of the glasses with their newly applied BNO tapes. After a few moments, the handholding was clearly unnecessary. Her mom commented “she seems to like it”. Greenwald, a pioneer of this treatment method describes two categories of patient responses to BNO; favorable and unfavorable.13 In the second unfavorable category the patients respond, “with great discomfort” and “a feeling of animosity toward the optometrist”. The first category, favorable response, is described by Greenwald in this way.
The first group of patients report some initial getting used to, then seem generally happy with the tapes. It is as if they were just waiting for someone to suggest something like this to them.
BNO success rate in converting esotropia to alignment has not been studied in cases like CJ in which there is a hyperopic component to the esotropia. It been reported to be 13 % among children with constant esotropia in the age range of 18 months through three years.4 The hyperopia status of these children was not reported. A likely prerequisite for amelioration of esotropia is a patient who functioned with bifoveal alignment for a good chunk of their early life, as did CJ. A unique feature of this case is the young age of the patient with attendant high neuroplasticity. Ostensibly, CJ’s brain was amenable to restoration of normal sensory fusion and / or the abnormal sensory fusion was not deeply embedded. BNO reset her vision so that she could return to functioning with manifest bifoveal alignment as she had for the first 15 months of life.
While BNO does not always convert esotropia to no manifest strabismus, its success may be defined at a lesser but meaningful level. It can improve sensory fusion as measured, for example, by major amblyscope 12 or vertical prism to alignment tests.12 The manifest esotropia does not resolve but the BNO improves the success rate of success rate of subsequent vision therapy, prism or eye muscle surgery. That BNO can be an effective treatment option for various types of esotropia is also published in a recent study by Zhao et al.14
Conclusions
BNO is a passive, viable, treatment method for esotropia that converted a young girl from esotropia to esophoria. Its prime mechanism is to occlude the fovea of the esotropic eye which suspends pre-existing abnormal sensory fusion. It is inexpensive and easily employed if the patient already requires glasses. It appears to have niche suitability for patients whose potential ocular alignment is prohibited by shallow abnormal sensory fusion and have divergence impetus in place. This article discussed and interpreted BNO strictly in a binocular vision paradigm. BNO is known to impact visual function in other ways 4,15 and those may have very well influenced the beneficial changes imparted to the girl in this case.
Conflict of Interests
The author declares that there is no conflict of interests regarding the methods and devices mentioned in the article.
