Change in objective bulbar redness and symptoms after refit of weekly and monthly lenses into a water-gradient daily disposable lens material
Purpose: The purpose of this pilot study is to identify if fine graduated differences in objective redness of the eye exist in a cohort of non-symptomatic contact lens wearers. The primary objective is the evaluation of change in bulbar redness when a non-symptomatic, 2-4 week contact lens wearer, is refitted to a Delefilcon A lens material. Secondary objectives include the determination of limbal redness, corneal and bulbar staining, and wearing comfort.
Material and Methods: 52 habitual, asymptomatic, full time soft contact lens wearers were enrolled in a multicenter study. At the baseline visit, bulbar and limbal redness were measured objectively using the Redness-Scan of the Keratograph 5M (K5M). Habitual lenses, lens care type, comfort ratings and staining data were captured at baseline visit. A wash out phase of 6 ± 1 days was conducted in which the subjects did not wear any lenses before Delefilcon A lenses were dispensed at visit 2 (V2) for a wearing period of 26 ± 5 days. A follow up visit was planned after 6 ± 1 days from V2 and a final visit after additional 20 ± 4 days. During visits 2, 3 and 4, the same objective measurements were carried out and corresponding subjective data was captured. ANOVA, t-test for paired samples, homogeneity test and Wilcoxon signed rank test were used for the statistical analyses.
Results: A total number of 49 complete data sets were successfully evaluated. Objectively measured bulbar redness decreased by 0.121 (p = 0.003) from the baseline compared to the final visit. In the same period, limbal redness reduced by 0.151 (p = 0.000). In addition, an increase from 36 at baseline to 47 at V4 grade 0 ratings regarding corneal staining, and from 32 to 39 regarding bulbar staining was found, respectively. The averaged comfort rating with habitual lenses was 79.7 ± 16.6 compared to the final visit 89.0 ± 10.8.
Conclusion: In the context of classic subjective grading habits which use fully grades in 1.0 steps, the objective Redness-Scan was able to detect finely graduated differences in the cohort of non-symptomatic wearers. The daily disposable test product delivers benefits to wearers in the form of reduced bulbar and limbal redness, reduced corneal and bulbar staining, and statistically and clinically increased contact lens wearing comfort.
Introduction
Beside subjective ocular sensations, the occurrence of redness is an important criterion, which helps contact lens wearers to notice, if their eyes are “healthy” or not. It is a common reason to consult medical help. For contact lens experts it is an important clinical safety parameter which needs an accurate diagnosis.
Redness can occur as a result of hyperaemia of the conjunctival and episcleral vessels due to an unspecific reaction to a number of factors.1,2 Possible reasons for redness, are diseases caused by soft contact lenses, e. g., Contact Lens Acute Red Eye (CLARE) 3–5, Contact Lens Related Peripheral Ulcer (CLPU) 6,7, Microbial Keratitis (MK) 8,9, Acanthamoeba Keratitis (AK) 10, Giant Papillary Conjunctivitis (CLPC) 11,12, as well as environmental, metabolic, chemical, toxic, allergic or mechanical effects.13 Furthermore, hyperaemia can be seen in a variety of grades within dry eye patients.14,15 So, age and gender are factors that should be considered, too.16
It is known that contact lenses are a barrier for oxygen reaching the cornea and conjunctiva. Especially contact lenses with a low Dk/t-value, that are worn over night, lead to an increase of bulbar and limbal redness.17,18,2 In contrast to that, silicone hydrogel contact lenses show only small impact to hypoxia.19 Mechanical impacts due to contact lenses, such as increased movement on the eye, can also lead to a higher level of bulbar and limbal redness.20
Secondary to allergic reactions, some ingredients in contact lens care solutions can increase ocular redness as well. For example the first generation mercury based disinfection molecule, benzalkonium chloride.21–23 Buffers seem to be relevant for ocular staining in nowadays lens care solutions.24,25 They adjust the pH-value but especially phosphate buffers are known to increase ocular redness.13 Because specific molecules can be absorbed by the lens material or in the lens case, which can be released on the eye to interact with the cornea and conjunctiva. Another possible irritant ingredient is Polyquat. Polyquat is an antimicrobial agent from the group of Quats. It is a long chain molecule and too big in relation to a pore of a contact lens. That´s why the uptake in the lens material is minimal. Polyquat has little interaction with the cornea and conjunctiva and does not lead to redness.26,27
For the evaluation of redness (and staining) of the eye a number of grading scales have been developed using classified photographs, drawn pictures or computer generated morphology.13 Examples of globally used grading scales are the Cornea and Contact lens research Unit (CCLRU) grading scale (Brien Holden Vision Institute) 28, the Efron grading-scale 13 and the JenVis grading-scale.29,30 Already in the year 1889 Müller described the distinction between bulbar and limbal redness, which is standard in most grading-scales nowadays.31 Murphy et al. reported an average bulbar redness grade of 1.9 (not validated CCLRU grading scale) units to be physiologically normal (mean age of the test group was 28 years).32 “A bulbar redness of greater than 2.6 units may be considered abnormal, and a change in bulbar redness of ≥ 0.4 units may be significant”.32 In an older test group, mean age of 45 years, a mean bulbar redness of more than 2.8 units and a mean limbal redness of more than 2.5 units is described as symptomatic.32,33
The problem of the printed scales is the lower precision due to subjective assessment 34, although this can be improved by using smaller grading unit divisions (e. g. 0.1 units).35 Furthermore, the same indication could be assessed differently using different grading scales.36,37 These problems can be avoided by objective methods, like the Redness-Scan with a multifunctional topographer (R-Scan Keratograph K5M, Oculus, Germany), which was used in this study. Firstly, the K5M classifies red, green, and blue colors in the captured image of the eye. By detecting the iris, lids and lashes the bulbar conjunctiva gets separated. After an automatical masking of the scleral vessels, the parts of red color with area and number of vessels are detected.38 By adjusting the focus precisely with a constant level of light during the measurement K5M shows a high reproducibility and a better inter observer repeatability than subjective interpreted grading-scales.39,40
Staining, can be detected using fluorescein and assessed by a grading scale. Based on subjective evaluation using a pictorial scale, the normal grade for corneal staining and conjunctival staining in healthy eyes is 0.5 (grade 0 - 4 in 0.5 steps).41,42 Contact lens wearers often show higher grades of staining.43,44 Staining below grade 2 can be tolerated.13,45 A comparison of non-contact lens wearers, hydrogel contact lens wearers, and silicon hydrogel contact lens wearers showed that the latter have significant more bulbar staining than the other groups.46 Especially the edge design of a lens is responsible for edge marks.47 Silicon-hydrogel-lenses with a water gradient material Delefilcon (Alcon, Fort Worth, USA) showed significantly less edge marks and staining than others.48
Besides redness and staining, subjective comfort is an important parameter. Ocular discomfort is the main reason for drop-out from contact lens wear.40,18,49 One possibility to reduce discomfort is a changeover to a daily disposable contact lens.50–52
The aim of this study is to assess, that a Delefilcon one day contact lens will reduce ocular redness in comparison to habitual 2–4-week soft lenses, when non-polyquad based contact lens care is used. Primary objective is the change in bulbar redness. Secondary objectives are limbal redness, corneal and bulbar staining and wearing comfort after the refit.
Material and methods
Subjects
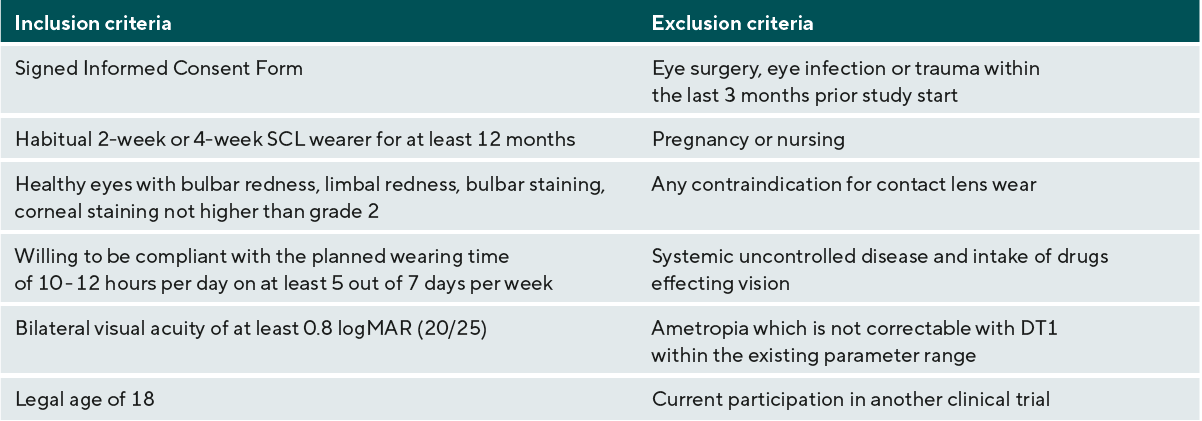
In this prospective open label designed pilot study a total of 52 asymptomatic soft contact lens wearers with spherical correction were enrolled. Inclusion and exclusion criteria are shown in Table 1. The sample size was calculated with 49 subjects based on subjectively determined data of ocular redness changes.18 Based on the habitually worn contact lens materials the subjects were allocated into either the hydrogel (group I-IV 53, n = 25) or the silicone hydrogel group (group V a, b, c 53, n = 24). All subjects used non-polyquad based multipurpose solutions and no peroxide solutions for their habitual lens care.
Test sites
Observers of two trained test sites (Optometrie Stefan Schwarz, Hildesheim, Germany and JENVIS Research, Jena, Germany) conducted the clinical evaluations. The study was stopped in March 2020 due to COVID 19 restrictions and continued after the first lock down. The ethical approval for the study was obtained by the Friedrich Schiller University in Jena, Germany. The study followed the principles of the Declaration of Helsinki and the Good clinical practice. Every subject signed the Consent Form after explanations and answering all questions about the study by the observer.
Techniques
Primary objective of the study was the evaluation of change in bulbar redness when a water gradient daily disposable silicone hydrogel lens (Delefilcon A) is refitted in 2–4-week contact lens wearers. Bulbar redness was measured with Keratograph K5M in 0.1 steps between grade 0 and 4 (Figure 1). The metric endpoint is clinically significant from a difference of 0.5 32 based on widely used pictorial scales.
The secondary endpoints were corneal and bulbar staining (grade 0 - 4 in 1.0 steps using the JENVIS grading-scale 2019 54) as well as limbal redness prior and after the refit (grade 0-4 in 0.1 steps measured with K5M). Furthermore, the subjective wearing comfort was assessed at every visit by using a visual analogue scale ranging from 0 (worst case) to 100 (best case).
Subjective refraction was performed by using an illuminated test-chart (type Polatest, Zeiss, Germany). The tolerated fitting criteria for movement and centration of the Delefilcon lens are shown in Table 2.
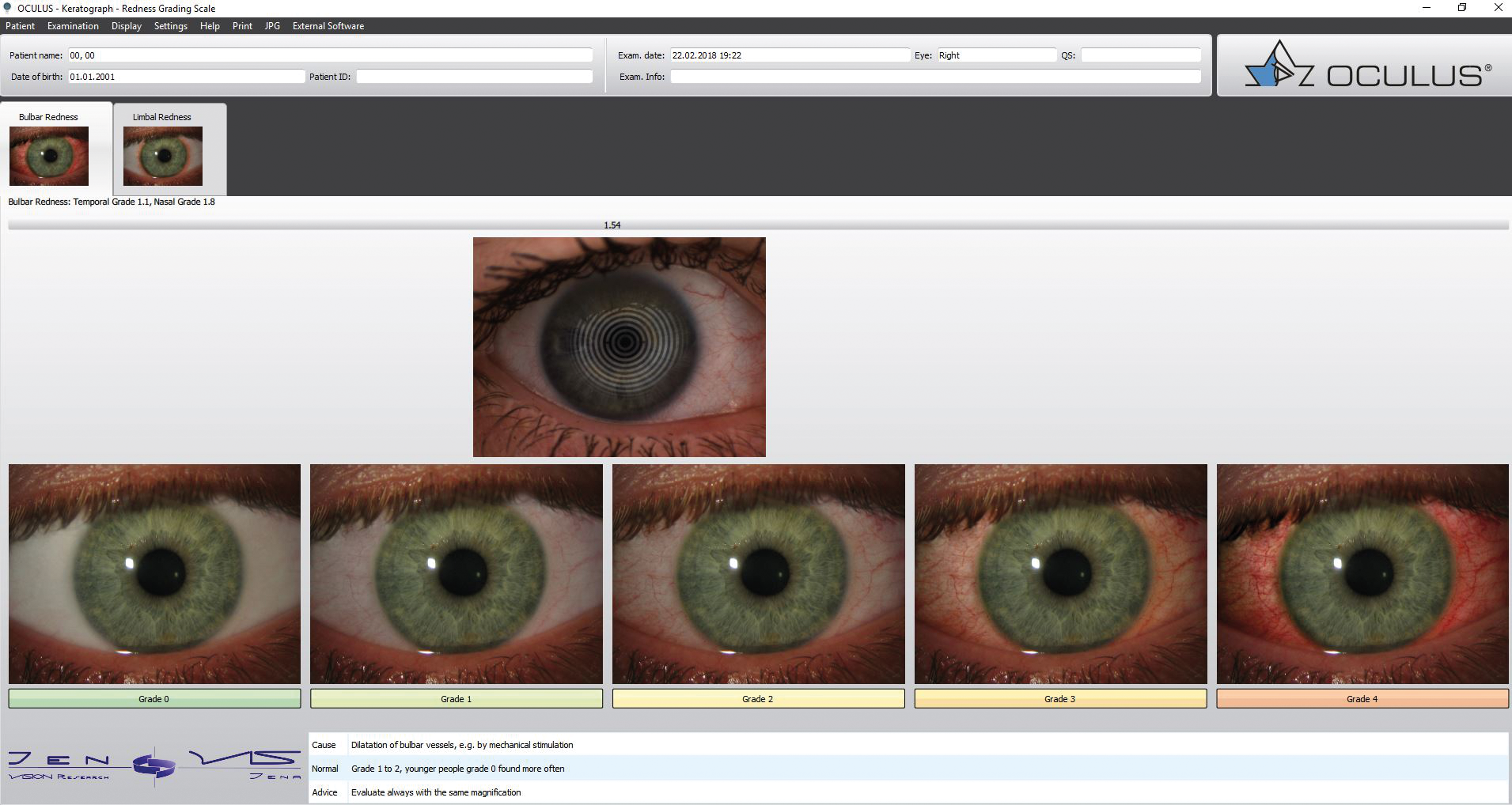
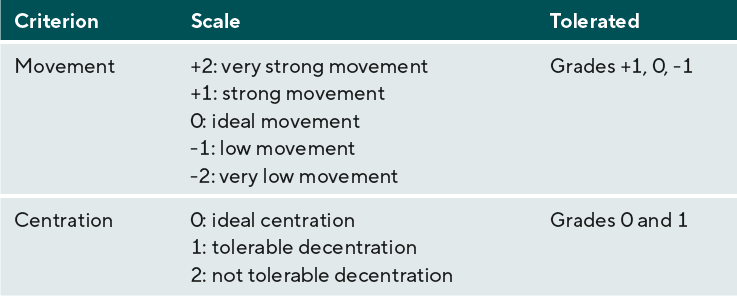
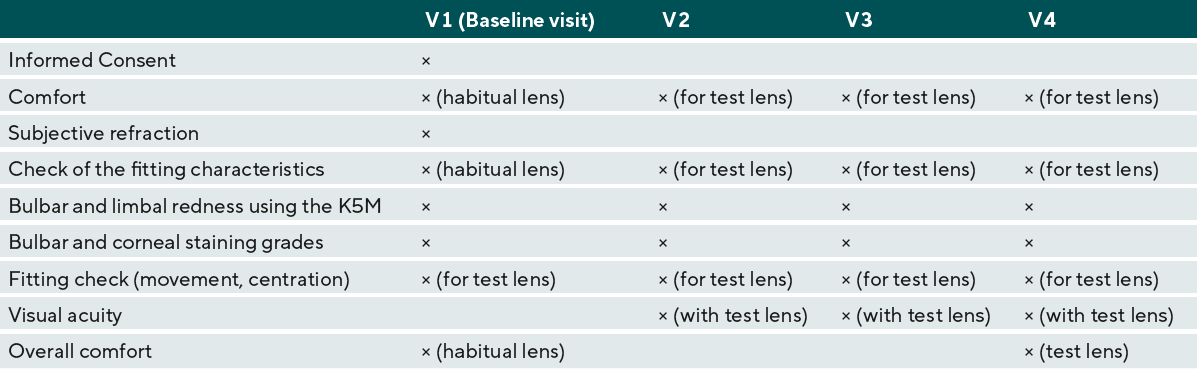
Figure 2 gives an overview about the planned study visits. At the Baseline examination (visit 1 / V1) the habitually used lens material and lens care solution were captured as well as demographical data and the duration of soft contact lens wear. Test persons had to wear their contact lenses at least 4 hours before the examination. This wearing time was documented and all follow up visits (V2 to V4) were made at the same contact lens wearing time. The date of the V1 examination was always arranged in the middle of the wearing period of the habitual lens. For monthly lenses, all lenses were examined after 2 of 4 weeks of wearing time (± 2 days), for biweekly lenses, all lenses were examined after 1 week of wearing time (± 1 day).
The baseline measurement included the Informed Consent, a comfort questionnaire about the habitual lens, a subjective refraction, the check of the fitting characteristics of the habitual lens (movement and centration), as well as bulbar and limbal redness using the K5M Redness-Scan, bulbar and corneal staining grades, and the fitting check for the Delefilcon A test lens (movement, centration, VA) to ensure that the test lens is suitable for the test person.
Participants underwent a wash-out phase of 6 ± 1 days of no contact lens wear before Delefilcon A lenses were dispensed at V2 for a wearing period of 26 ± 5 days. The following parameters were collected at V2: comfort, bulbar and limbal redness, bulbar and corneal staining, and refraction. Movement, centration, and visual acuity were assessed after dispensing the test lenses. After another DT1 wearing period of 6 ± 1 days the third visit (V3) included the same assessments as V2. So did the final visit (V4) after 20 ± 4 days from V3. At visits 1 and 4 overall comfort with the habitual SCL respectively the Delefilcon A test lens were collected (Table 3).

Statistical analysis
For the statistical analysis the program IBM SPSS Statistics (Version 24) was used. Only data of the right eyes were considered for analysis. Normal distribution was tested by the Kolmogorov-Smirnov-Test. Bulbar and limbal redness were analyzed by the paired t-test and the Anova for repeated measurements. The ordinal endpoints of staining were analyzed by homogeneity test. Furthermore, the exploratory endpoint subjective wearing comfort was assessed at every visit by using a visual analogue scale ranging from 0 (worst case) to 100 (best case). It was analyzed by Wilcoxon signed rank test.
Results
Fifty (35 females, 15 males; mean age 31.4 ± 10.6 years) of 52 asymptomatic soft contact lens wearers with spherical correction completed the study. Two subjects discontinued due to time conflicts. One subject missed visit 3 due to a COVID 19 quarantine. So, 49 complete data sets were successfully evaluated.
Redness
Data of bulbar and limbal redness showed a normal distribution at all visits (bulbar redness V1, V2, V3 p = 0.200, V4 p = 0.174; limbal redness V1 p = 0.037, V2 p = 0.200; V3 p = 0.043; V4 p = 0.032).
Bulbar redness
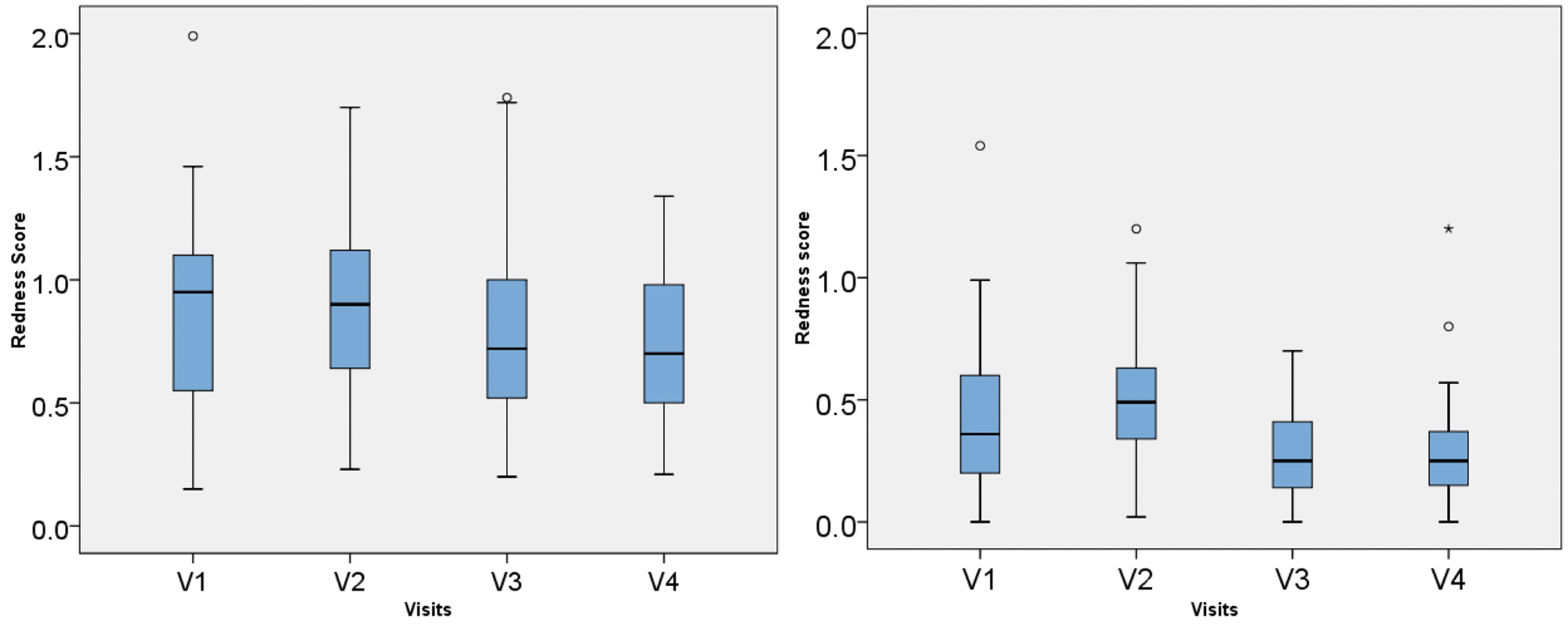
The results regarding bulbar redness are graphically shown in Figure 3. Mean bulbar redness scores were statistically significant different between all four visits (Anova repeated measurements; F = 10.538, p = 0.000, ηp2 = 0.180, n = 49; sphericity assumed with Mauchly-W = 0.820, p = 0.0099) as well as between V1 and V4 (paired t-test; difference 0.121; p = 0.002). The Post hoc test (Bonferroni) shows the significant differences of bulbar redness between V1 and V4 (p = 0.013), V2 and V3 (p = 0.000) and V2 and V4 (p = 0.000).
A statistically significant lower grade of bulbar redness between V1 and V4 appeared in the subgroup of hydrogel lens wearers (paired t-test: difference of 0.110 / p = 0.012). The Anova for repeated measurements indicates differences in bulbar redness between all four visits (F = 4.361, p = 0.007, ηp2 = 0.154, n = 25) (see Table 4). The Post hoc test (Bonferroni) shows that the significant difference lies between V2 and V4 (p = 0.004). No statistically significant difference in bulbar redness between visits 1 and 4 exists after refit from a soft silicone hydrogel contact lens (paired t-test: difference of 0.133 / = 0.050) (see Table 4). Nevertheless, the Anova indicates differences between all four visits (F = 7.872, p = 0.001, ηp2 = 0.255, n = 24). The Post hoc test (Bonferroni) shows the significant differences of between V2 and V3 (p = 0.000) and V2 and V4 (p = 0.004).
Limbal redness
As seen in Figure 4, limbal redness shows a statistically significant decrease between V1 and V4 (paired t-test, difference of 0.151 / p = 0.000). The Anova for repeated measurements (Greenhouse-Geisser correction with Mauchly-W = 0.602, p = 0.000) shows moderate differences between limbal redness at the four visits (F = 25.300, p = 0.000, ηp2 = 0.345, n = 49) (see Table 4). The Post hoc test (Bonferroni) show the significant differences between V1 and V3 (p = 0.000), V1 and V4 (p = 0.001), V2 and V3 (p = 0.000) and V2 and V4 (p = 0.000).
Statistically significant lower grades of limbal redness were also found after refit from a soft hydrogel contact lens (paired t-test: difference of 0.172, p = 0.000) and from a soft silicone hydrogel lens (paired t-test: difference of 0.130, p = 0.048). In the subgroup of hydrogel lens wearers, the Anova shows significant differences between the four visits (F = 22.816, p = 0.000, ηp2 = 1.276, n = 25) with main differences between, V1 and V4 (p = 0.001), V2 and V3 (p = 0.000) and V2 and V4 (p = 0.000). In the silicon hydrogel group, the significant differences (F = 7.545, p = 0.001, ηp2 = 0.773, n=24) can be stated between V2 and V3 (p = 0.000).

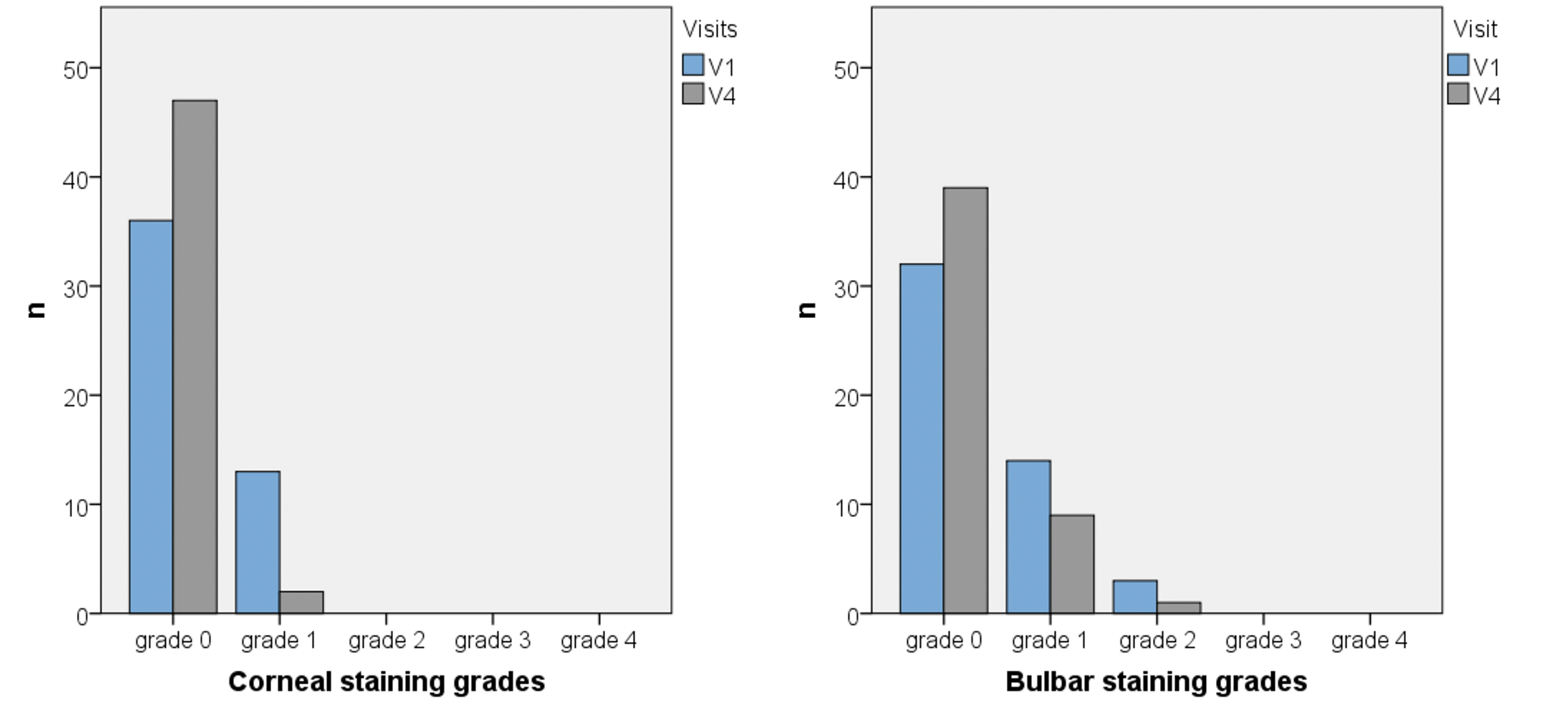
Staining
Corneal and bulbar staining were analyzed in addition to ocular redness. The overall analysis (homogeneity test (summetry test of Bowker)) shows statistical significant differences in corneal staining grades between V1 and V4 (p = 0.001). Figure 5 illustrates that the number of grades 1 reduced and the number of grades 0 increased in comparison to visit 1. In bulbar staining no significant differences can be found between staining grades (p = 0.050). Figure 6 shows, that the number of grades 0 to 2 is nearly the same
at V1 and V4.
The subgroup analysis shows statistically significant lower grades of corneal (p = 0.014) and bulbar staining (p = 0.046) in the hydrogel group. In the subgroup of previous silicon hydrogel soft contact lens wearers only corneal staining shows a reduction between V1 and V4 (p = 0.025) (see Table 5).
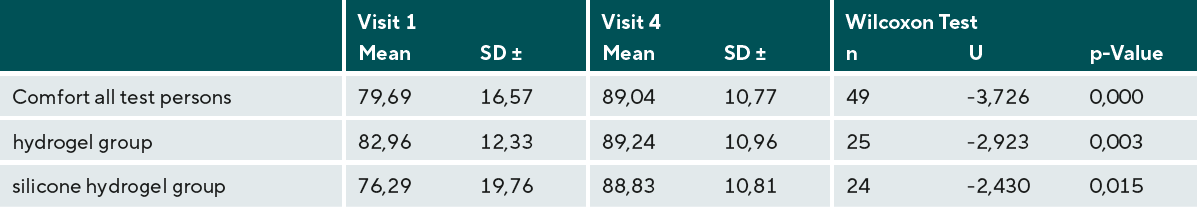
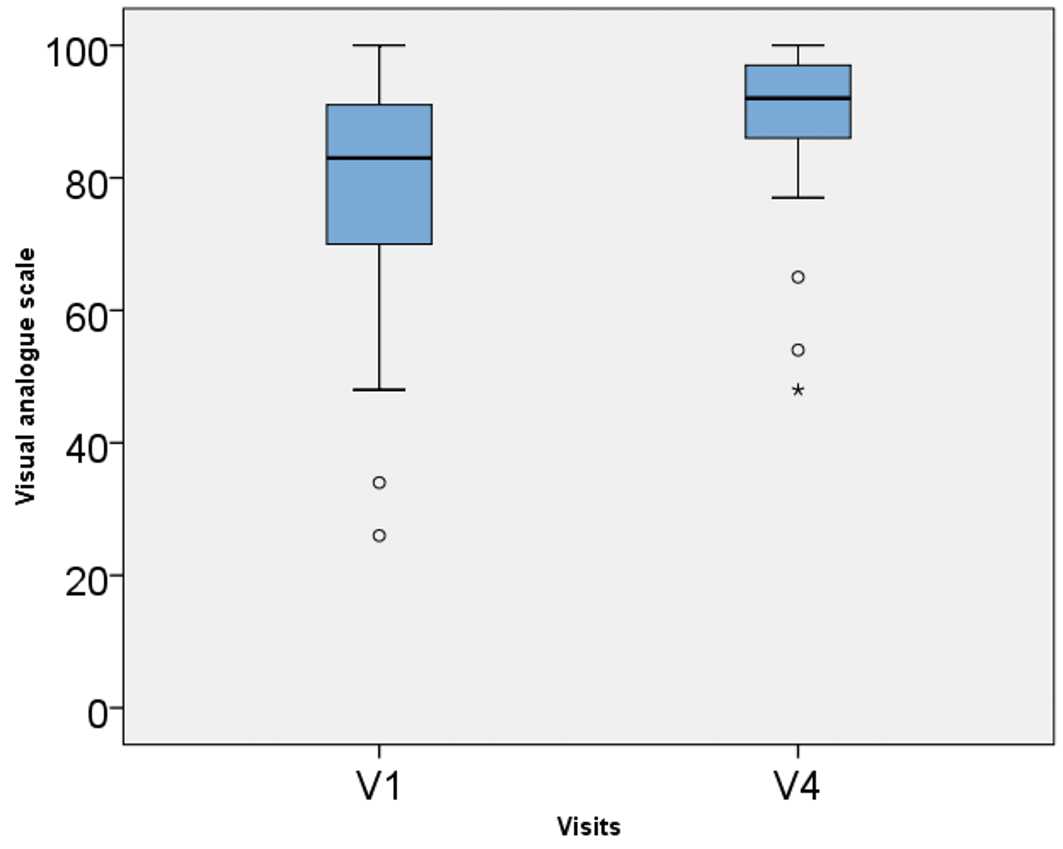
Comfort
The exploratory endpoint was the subjective comfort. The ratings captured at V4 were higher than the ratings with the habitual lens at V1. As shown in Figure 7, the range of responses were much smaller after wearing the test lenses. Overall comfort is rated significantly higher with Delefilcon A after refit from another soft contact lens (p = 0.000), regardless of the subgroup (hydrogel subgroup: comfort p = 0.015; silicone hydrogel subgroup: comfort p = 0.003) (see Table 6).
Discussion
This study indicates that the grade of bulbar redness is (with a difference of 0.121 between V1 and V4) statistically significant lower after refit to a daily disposable silicone hydrogel contact lens (DT1) for non-symptomatic 2–4-week CL-wearers. Although in context of the classic subjective linear grading habits (which use grades in 1.0 steps), this difference is small. The K5M can detect fine graduated differences in the cohort of non-symptomatic wearers, which show low physiological redness scores. Similar results are shown by the secondary endpoints of limbal redness with a difference of 0.151 between V1 and V4. In addition, an increase from 36 at baseline to 47 at V4 grade 0 ratings regarding corneal staining, and respectively from 32 to 39 regarding bulbar staining was found.
The small objective differences seem to be not clinically relevant. But the benefits of the refit to the non-symptomatic wearers in this study allow the assumption, that the positive influence on symptomatic wearers with higher grades of redness and staining grades could be much higher. The objective results are supplemented by the exploratory endpoint of subjective wearing comfort. It shows higher ratings after the refit with an increase of 9.5 points.
Studies have already proven a significant decrease of bulbar and limbal redness after refit to a silicon hydrogel contact lens.56,18,57–59 But none of these study designs used an objective measurement device for the ocular redness determination, like the R-Scan (K5M), which shows a high reproducibility under constant environmental measurement conditions and use by the same examiner.40 Furthermore the R-Scan tolerates small uncertainties of the measurement, because of an imprecise focus.40 Dumbleton et al.18 identified a lower bulbar redness (p < 0 .001) and limbal redness (p < 0.001) after refit from successful daily or monthly hydrogel lens wearers to monthly silicone hydrogel contact lenses. Redness was measured by a 0–100-point score. No limitations regarding the contact lens care solution were set. Multi-purpose solutions as well as Peroxide solutions were allowed in this study as habitual lens care systems at the baseline visit. In contrast to that Riley et al.59 refitted symptomatic hydrogel contact lens wearers with redness greater or equal grade 2 to two-week silicone hydrogel lenses. Redness was evaluated by a 0–4-point score. Bulbar redness (p < 0.001) and limbal redness (p < 0.002) decreased significantly. A number of studies included the parameters of corneal and bulbar staining, too.57,56,59,58 Dillehay and Miller 58 described a significant decrease in corneal and bulbar staining after refit from low-Dk/t-value contact lenses to silicone hydrogel contact lenses. Furthermore, Hickson-Curran et al.50 confirmed in a retrospective study a number of advantages of daily disposable contact lenses, such as reduced dryness and staining.
All the mentioned publications are in agreement to the described study. Nevertheless, no comparative study with a refit to Delefilcon A contact lens was found. This study confirmed that the test lens (Delefilcon A) improves ocular redness in comparison to habitual soft contact lenses, especially when non-polyquad based contact lens care was used along the habitual lenses. The test lens (Delefilcon A) delivers benefits to wearers in form of reduced bulbar and limbal redness, reduced corneal and bulbar staining, and increased wearing comfort.
Despite the fact that the primary endpoint was captured in an objective way, the investigators were not masked. This is a limitation of the study. It should be also taken into account that new lenses are likely to be better evaluated regarding comfort and vision. This limitation could have been avoided by a more complex study design. However, the necessary resources were not available.
Conclusion
The study shows that it is possible to capture bulbar and limbal redness data via an objective measurement approach. The data demonstrate a statistically significant decrease in limbal and bulbar redness, as well as subjectively determined corneal and bulbar staining after refit to a daily disposable water-gradient silicone hydrogel contact lens (Delefilcon A) in non-symptomatic 2–4-week CL-wearers. The benefits after refit include a statistically and clinically increase in subjective wearing comfort. The objective differences, detected by the K5M, are statistically relevant, even if the cohort includes non-symptomatic wearers. In symptomatic wearers the benefits of refit are supposed to be higher, which should be researched in subsequent studies.
Conflict of interest
The authors declare that there is no conflict of interests regarding the methods and devices mentioned in the article.
Acknowledgments
The investigator study was funded by Alcon (IIT# 43410197).
Figures: Copyright by Sebastian Marx
