A tectonic eccentric penetrating sclerokeratoplasty à chaud followed by partial conjunctival flap surgery as treatment for a peripheral perforated ulcer in Wegener‘s disease
Purpose: This case report describes the surgical treatment of a 70-year-old female patient with a massively reduced general condition, painless redness associated with a foreign body sensation, sensitivity to glare and increasing visual impairment of the right eye.
Material and Methods: The clinical findings of the morphological anterior segment showed a most likely sterile infection with a limbus-parallel corneal stromal melting larger than 6 mm. The suspected granulomatosis with polyangiitis (Wegener’s disease) was confirmed in the extended autoimmune serology. The patient initially underwent a perforating tectonic eccentric sclerokeratoplasty à chaud. The aim was to preserve the eye. Eighth months after the eccentric perforating sclerokeratoplasty, a new perforation developed, so a partial conjunctival flap was then added.
Results: The eye could be preserved because of the perforating tectonic eccentric sclerokeratoplasty à chaud and the additional partial conjunctival flap. As expected, the surgery did not improve vision but stabilised the eyeball.
Conclusion: Patients with Wegener’s disease involving the eye have the worst ocular prognosis, as they more frequently develop necrotising anterior scleritis as well as a loss of visual acuity and peripheral ulcerative keratitis. The current therapeutic approach initially involves surgical treatment of the corneal melting and, of course, stabilisation of the eyeball in the case of perforation. Partial or complete conjunctival flaps are used for severe, chronic and painful corneal surface problems when all other treatment options have failed
Case presentation
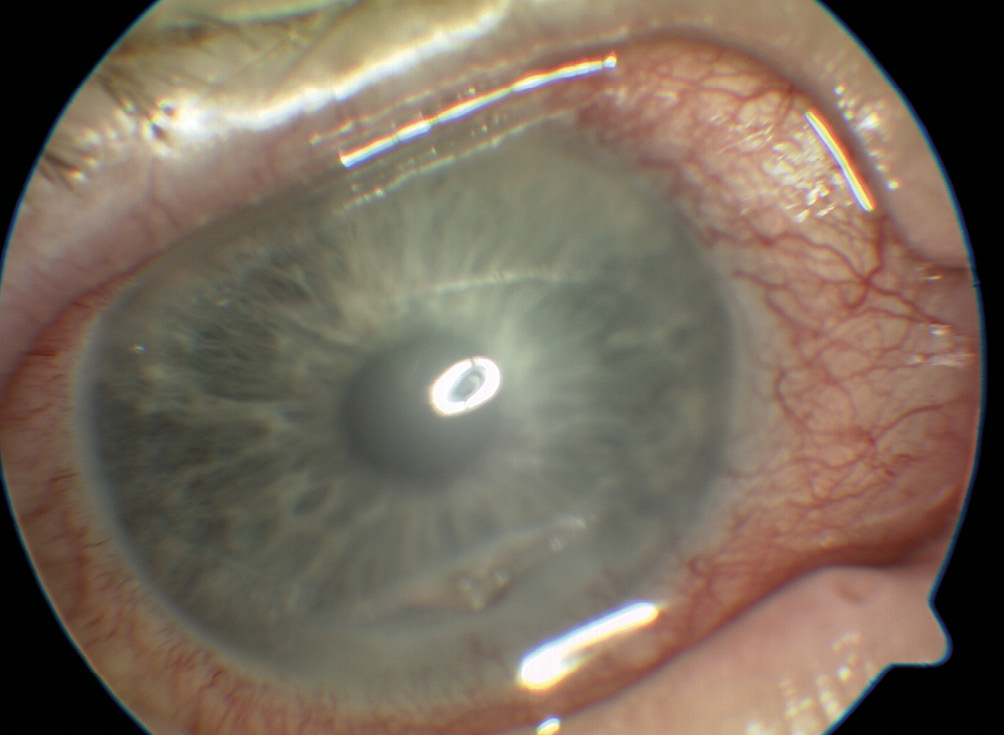
In August 2019, a 70-year-old female patient came as an emergency case to our outpatient clinic in a massively reduced general condition with painless redness accompanied by a foreign body sensation, sensitivity to glare and increasing visual impairment of the right eye. A perforated corneal ulcer over 6 mm in size was found close to the limbus in the lower circumference (Figure 1).
The routine laboratory examination revealed anaemia, an increased erythrocyte sedimentation rate (ESR) of 70 mm/h and increased renal retention values with a creatinine value of 1.55 mg/dl and a significantly reduced glomerular filtration rate (GFR) of 38 ml/min. The suspected diagnosis of granulomatosis with polyangiitis (Wegener‘s disease) was confirmed in the extended autoimmune serology with an increased anti-neutrophil cytoplasmic antibody (c-ANCA) with a ratio of 1 : 640 specifically against the enzyme proteinase 3.1,2
Therapeutic surgical procedure
The patient underwent a perforating tectonic eccentric sclerokeratoplasty à chaud under intubation anaesthesia (Figure 2).3
First, the eye globe was stabilised via the anterior chamber using highly viscous hyaluronic acid after performing a paracentesis. The conjunctiva was then opened parallel to the limbus in the area of the marginal ulceration and the sclera was exposed 3 – 4 mm away from the limbus. A precision diamond knife was then used to perform a 2 – 3 mm scleral incision with a 300 µm depth and the sclera was lamellarised so that the ciliary muscle insertion at the scleral spur and the episcleral venous system remained as intact as possible.
A precision diamond knife was then used to cut into the intact corneal stroma to a depth of approx. 400 µm and at a position of 1 – 2 mm next to the marginal ulceration. This preparation produces a semi-ellipsoidal corneoscleral disc.
The donor corneoscleral disc with a scleral base of approximately 2 – 3 mm was clamped in an artificial anterior chamber and filled and stabilised with highly viscous viscoelastic. A precision diamond knife was then used to make an eccentric incision approx. 400 µm deep and approx. 0.25 – 0.5 mm larger than the recipient‘s corneal incision. The semi-ellipsoidal preparation was removed from the anterior chamber and cut corneally and sclerally with Vannas scissors. On the recipient, this was also done corneally with Vannas scissors, and the incision with curved corneal scissors was made at the corneoscleral junction according to Castroviejo.4,5
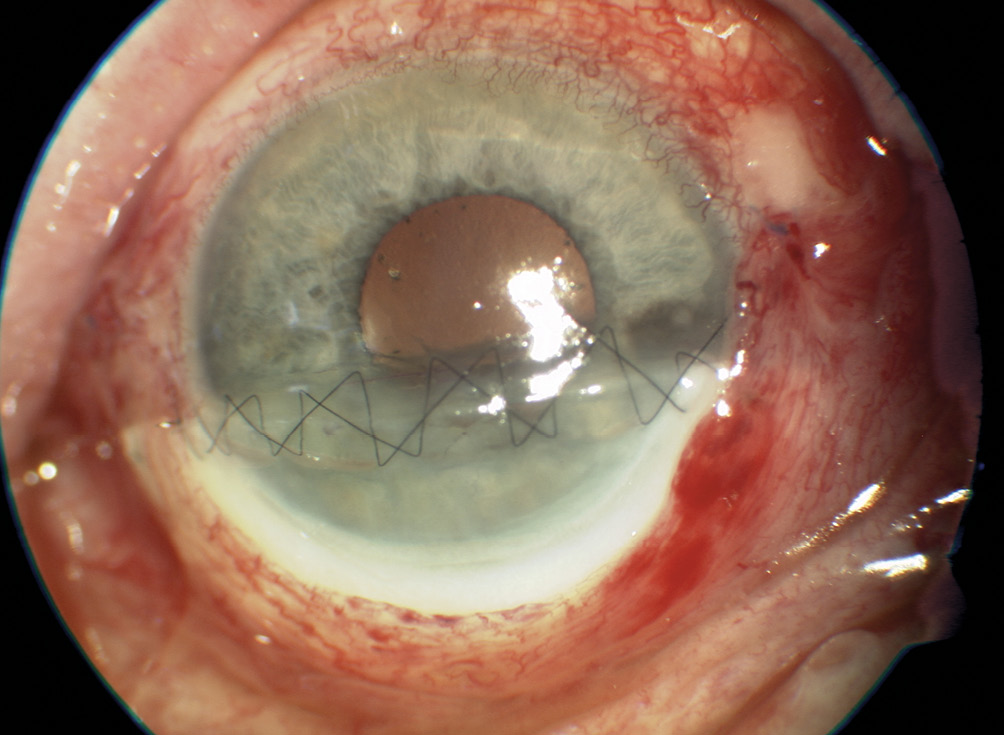
The corneoscleral graft was adjusted in the area of the limbus and the sclera with multiple 10-0 nylon sutures. This adjustment was performed using a continuous 10-0 nylon suture in the area of the corneal incision edge. The final conjunctival closure was performed using two single Vicryl 8-0 sutures.6,7
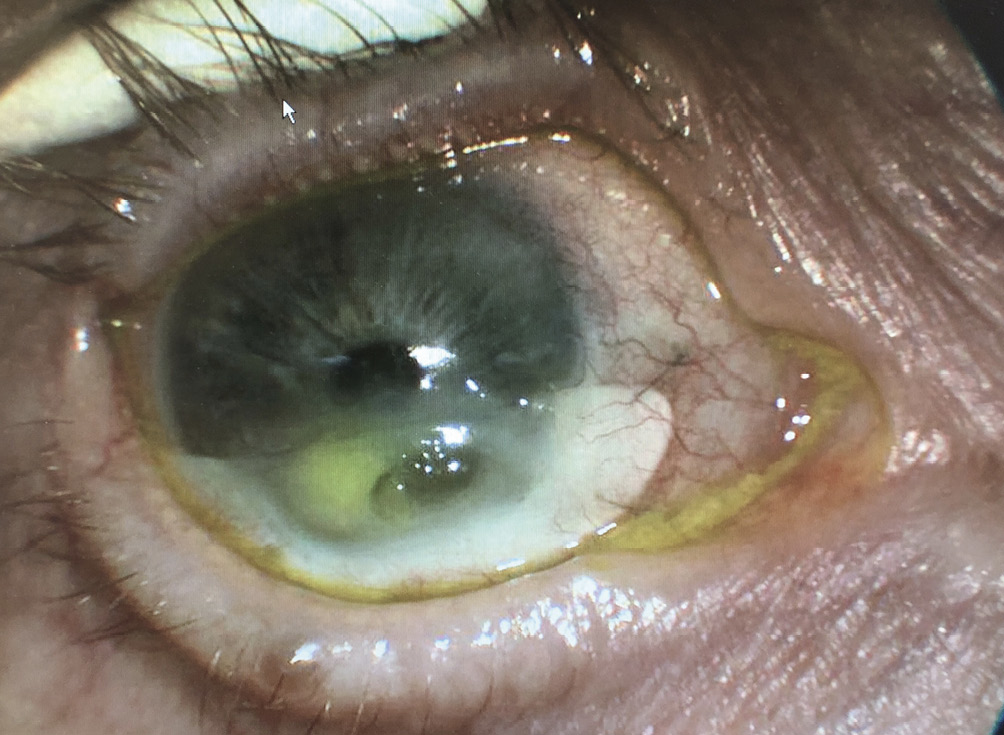
The continuous nylon sutures were removed after six months. In the eighth month, a new perforation formed
(Figure 3). A partial conjunctival flap was then added.
The aim of partial or complete conjunctival flap is to achieve permanent coverage of the corneal surface. To achieve this, a conjunctival flap must be pulled over the cornea partially or completely as tension-free as possible and then anchored stromally or at the limbus until the subconjunctiva has grown together with the diseased areas of the cornea. Nowadays, the Gundersen technique is generally used for this.8,9
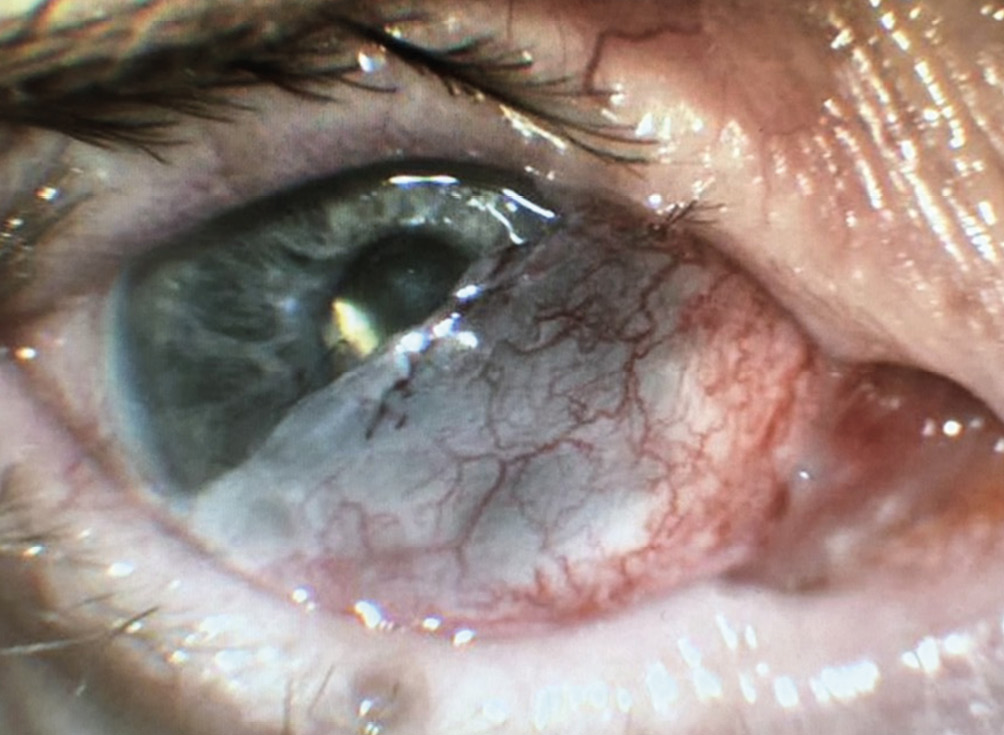
In partial conjunctival flap surgery, the previously mobilised conjunctiva is anchored intrastromally with a continuous nylon 10-0 suture approximately 1 – 2 mm from the corneal pathology after epithelial abrasion (Figure 4).
The continuous suture can usually be removed after 4 – 8 weeks. Until then, the underside of the conjunctiva is firmly attached to the abraded corneal surface. To ensure a pleasing appearance, either a flat ocular prosthesis (epithesis) or an iris print contact lens should be fitted after 4 – 6 weeks
Discussion
Granulomatosis with polyangiitis (Wegener‘s disease) can occur unilaterally or bilaterally; patients between their 50s and 70s are more frequently affected. Clinical findings in the early stages range from yellowish to greyish nodular lesions of the sclera close to the limbus and extending to the equator without vascular congestion, which grow, necrotise and conglomerate as the disease progresses. If the nodular changes are located directly at the limbus, perforation into the anterior chamber may occur. Other possible complications that can occur with all forms of scleritis are loss of visual acuity and associated keratitis. Concomitant anterior uveitis occurs in approximately 30 % of patients with scleritis (anterior and posterior). Wegener‘s disease may affect the eye in 28 – 60 % of cases. Patients with Wegener‘s disease involving the eye have the worst ocular prognosis, as they are more likely to develop necrotising anterior scleritis, loss of visual acuity and peripheral ulcerative keratitis. As soon as the diagnosis of Wegener‘s disease is clinically and serologically confirmed at the immune level (c-ANCA with target antigen proteinase 3; sensitivity is 85 – 90 % and specificity 95 %), stage-appropriate immunosuppressive therapy should be initiated immediately. If left untreated, the mortality rate is approx. 50 – 80 % within one year. In the localised stage, therapy is carried out with co-trimoxazole (combination of 160 mg trimethoprim and 800 mg sulfamethoxazole) in combination with low-dose prednisolone. In the generalisation stage, treatment is performed with cyclophosphamide (dosage 2 mg/kg of body weight) and high-dose prednisolone (dosage 1 mg/kg
of body weight). The 5-year survival rate with treatment is approx. 85 %.1,2 The clinical findings of the morphological anterior segment showed a most likely sterile infection with a limbus-parallel corneal stromal melting larger than 6 mm. In such an initial situation, it must also be remembered that this type of change can occur in the context of a lethal vasculitis.
The current therapeutic approach initially involves surgical repair of the corneal melting and, of course, stabilisation of the eyeball in the event of a perforation. As eccentric tectonic sclerokeratoplasties in open eyes can be extremely difficult to operate on and are performed extremely rarely, they are not part of the everyday practice of a cornea specialist and should be treated in specialised centres if necessary. There is no real standard procedure for this type of surgery. The size and localisation of the sclerokeratoplasty must be individually adapted in each case. Important in the operation is the lamellar superficial dissection of the scleral part with the aim of keeping the ciliary muscle insertion at the scleral spur, the trabecular meshwork and the episcleral venous system as intact as possible. Disrupting the drainage system over 4 – 5 hours could actually lead to postoperative secondary glaucoma. Finally, the patient must also be informed about the prognosis of a reduced visual acuity. The patient must understand that this type of surgery is not intended to improve vision, but to stabilise the eye globe and “save” the eye. Where applicable, an optical penetrating keratoplasty could be performed in a quiet interval as a vision-improving measure.
Partial or even complete conjunctival flap surgeries are performed much less frequently nowadays than in previous decades. They are now almost only indicated for chronic and painful corneal surface problems that require a permanent solution. These chronic surface problems include neurotrophic keratopathy, corneal ulceration processes with a poor or non-existent healing tendency and an unfavourable host cornea, corneal melting processes in deteriorating patients, inadequate aftercare options and painful keratopathia bullosa. Prior to the actual surgical procedure to cover the conjunctiva, all patients generally undergo weeks to months of outpatient and inpatient treatment for chronic, therapy-resistant surface changes and pain symptoms as well as underlying systemic diseases such as diabetes mellitus, Parkinson‘s disease or sleep apnoea.
We must consider the triggering pathogenetic factors and try to eliminate them in the treatment of these chronic corneal surface pathologies. Intensive collaboration with neurologists, diabetologists, internal medicine specialists, oncologists and rheumatologists is essential to adapt and, if possible, optimise systemic treatment.
The amniotic membrane plays a crucial role in the treatment of chronic surface problems. It serves as a basement membrane substitute and should act as a guide rail for epithelial growth. In the case of wound healing disorders, it promotes the proliferation and migration of epithelial cells and supports the all-important cell adhesion. Last but not least, the superficial inflammatory reaction and corneal melting are reduced, since the amniotic membrane stroma contains proteinase inhibitors.
Tarsorrhaphy is also a proven treatment option for chronic persistent epithelial defects. Alternatively, a botox injection into the upper eyelid levator palpebrae superioris muscle can be performed to create a ptosis.
Partial or complete conjunctival flaps are used for very severe chronic surface problems when all other treatment options fail. They represent an overall low-complication surgical option that shortens intensive, lengthy and extremely straining surface treatments. The aim is to calm the surface pathology and achieve no to little irritation in the eye. The only alternative is an evisceratio bulbi or enucleatio bulbi.
These thoughts on the treatment of corneal surface problems using conjunctival flaps were already very clearly presented by Gundersen in his 1958 publication.8 He considers the basic prerequisite to be an intact conjunctiva that has not previously been surgically altered or scarred. The most important step is the careful dissection of the conjunctiva. It must be carefully separated from the Tenon without causing conjunctival perforation, particularly in the centre. As soon as central holes occur in the conjunctival flap, these will retract and grow over time, rendering the coverage effect useless. Furthermore, careful epithelial abrasion is required, as otherwise adhesion and the subsequent fusion between the subconjunctiva and the corneal surface will not occur. In these cases, the conjunctival flap, whether partial or complete, will retract again. Once the conjunctiva has completely retracted, a new covering in a subsequent operation will only be partially successful, as there will be no permanent adhesion.
In approximately 5 % of cases, small circumscribed epithelial inclusion cysts may occur, which can be removed without difficulty if necessary. Mild blepharoptosis is described in approximately 7 % of cases. The cause of this narrowing of the palpebral fissures is probably in the upper fornix if fornix shortening or scarring has occurred after surgery.10,11,12
To ensure a pleasing cosmetic appearance, either a flat ocular prosthesis or an iris print contact lens should be fitted after 4 – 6 weeks. Patients tolerate both very well and are generally very satisfied with the cosmetic result, especially as the bulbus motility is normal compared to an enucleation.
Conflict of interest
The authors have no conflict of interest with regard to the methods and devices mentioned in the article.
A New Technique of Harvesting Freehand and Horseshoe Tectonic Grafts. Cornea, 34, 1519–1522.
