An empirical survey of the Preference use of filling solutions for scleral lenses by practitioners in Austria, Germany and Switzerland
Purpose: This study examines the use, distribution, and selection criteria of scleral lens (SCL) filling solutions among practitioners in German-speaking countries. It aims to provide an overview of advised and available products, regional preferences, and factors influencing solution choice.
Material and Methods: An online survey was conducted from November 13 to December 31, 2023. Data collected included participants’ filling solution preferences, experience with SCLs, and anonymous demographic information. A total of 121 complete responses were analyzed to identify usage Patterns and regional differences.
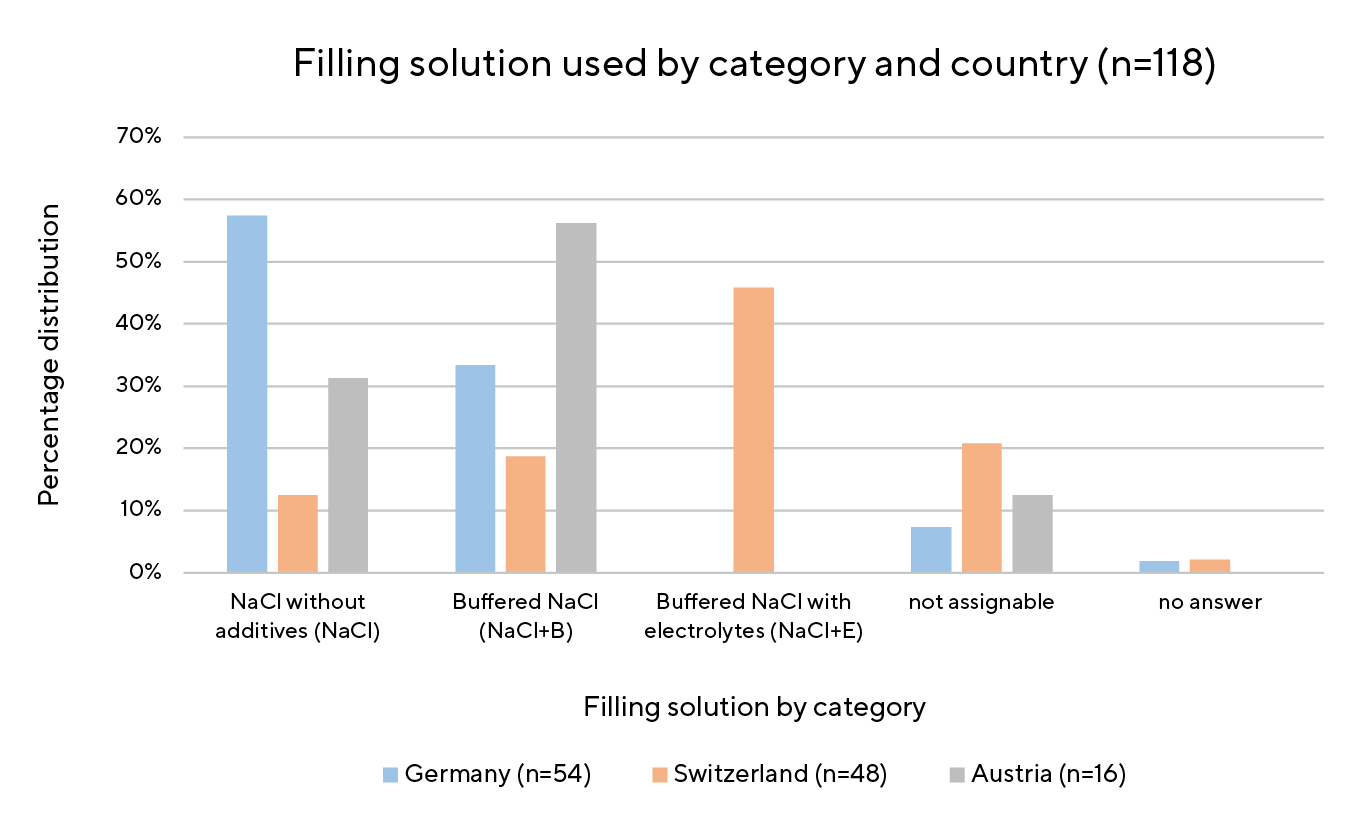
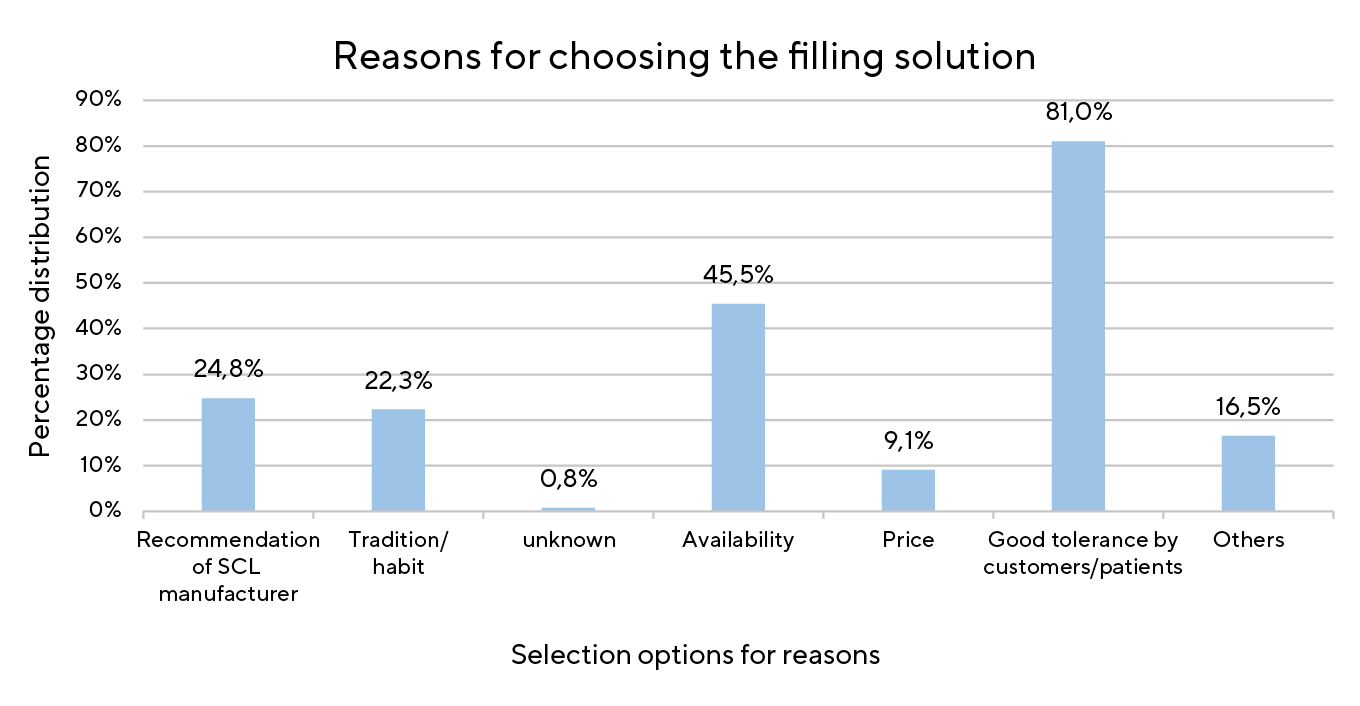
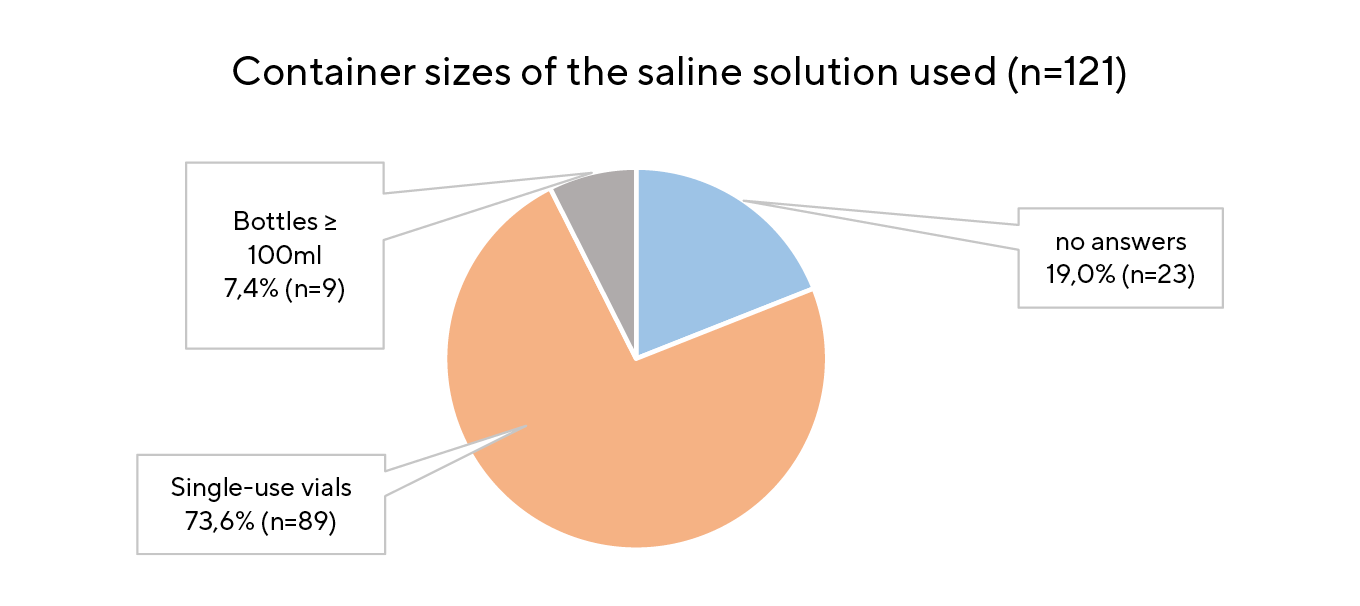
Results: Of 121 respondents, 118 were from Germany, Austria, or Switzerland, three from other countries. Seventeen different filling solutions were reported, eight of them accounted for 89.0 % of all responses. Products mentioned fewer than four responses were grouped under “Others”. The eight most common solutions were categorized into three types: isotonic sodium chloride (NaCl), saline with buffers (NaCl + B), and saline with buffers and electrolytes (NaCl + E). Regional trends emerged: In Germany (n = 53) NaCl is predominantly used; in Switzerland (n = 48) NaCl + E is preferred, while Austrian practitioners (n = 16) favored NaCL + B. Main selection criteria were good patient tolerability (81.0 %), availability (45.5 %), and SCL-manufacturer recommendation (24.8 %). Most participants (73.6 %) used single-use, preservative-free saline vials.
Conclusion: Several types of filling solutions exist. Most practitioners are satisfied with their current choice and only change when there are supply issues or ocular side effects, such as midday fogging (MDF). NaCl + E may delay or Prevent MDF and enhance subjective comfort, especially for patients with compromised corneas. Using NaCl + E, particularly in Germany, could improve outcomes for certain scleral lens patients.
Introduction
Scleral lenses (SCL) hold a unique position in the contact lens market. Originally developed in the late 19th century as waterfilled glass shells to improve vision, their use was initially limited to therapeutic applications for corneal anomalies.1,2 Over the past two decades, advancements in materials and manufacturing process have experienced a revival. In particular, the introduction of High Gas Permeable (HGP) materials has improved oxygen permeability and comfort.1,3
In contrast to corneal lenses, SCL completely bridge the cornea and rest on the scleral conjunctiva. Isotonic, preservative-free saline fully fills the space between the posterior lens surface and the cornea.4,5 The fluid reservoir (FR) remains in direct contact with the cornea and the tear film for several hours, providing continuous hydration and contributing to the correction of corneal irregularities. In cases of ocular surface disease (OSD), it also protects the cornea from external factors and mechanical friction.5,6,7
Besides optimal oxygen supply, proper lens care is essential for ocular health and comfort. Saline and contact lens care products must meet strict standards to ensure safety and compatibility. Key criteria include isotonicity (matching tear osmotic pressure), isohydric conditions (physiological pH value), sterility, chemical stability, and a refractive index close to that of the tear film (approximately 1.336).2,8,9
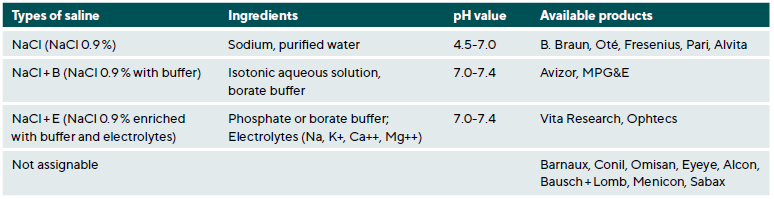
For scleral lens wearers, nonpreserved saline solutions in singleuse vials are highly recommended to minimize the risk of infections.3,5 Basically, three different types of filling solutions are offered and used: Isotonic saline (NaCl), pH value 4.5-7.0 10, buffered saline (NaCl + B), contains borate or phosphate buffer 11 and, buffered saline with electrolytes (NaCl + E) like sodium (Na), potassium (K+), calcium (Ca++), and magnesium (Mg++).12 pH value of NaCl + B and NaCl + E ranges from 7.0 – 7.4 which corresponds to the pH value of the tear film of a healthy eye (7.4 ± 0.2).8
Electrolytes and buffers play an important role in maintaining the stability and comfort of filling solutions and could improve the wear properties of SCL. Electrolytes help mimic the composition of natural tears while buffers, such as phosphates and borates, regulate pH value balance and reduce irritation.8
Buffers are also used in ophthalmics and artificial tears and are able to neutralise small amounts of acids and bases. In addition to borate and phosphate, commonly used buffers are citrate and tromethamine (TRIS).8,13
A major challenge for SCL users is Midday Fogging (MDF), a clouding of the FR that reduces visual clarity.7,14-19 MDF occurs minutes to hours after SCL insertion.15,16 Studies indicate that 20–46 % of SCL wearers are affected by this problem.14,15,18 Opacity is linked to cellular debris, lipids, proteins and leukocytes.14-16 Removing and refilling the lens is currently the most effective way to resolve the issue.17,18,19
Schornack at al. found no direct correlation between MDF and demographic characteristics such as age, sex, and ethnicity.14 Research indicates that patients with MDF often experience dry eye symptoms such as redness and irritation.18
Some studies show that electrolyte-enriched solutions improve subjective comfort and reduce these symptoms, though their impact on MDF remains inconclusive.16,17 Despite studies, there are still no clear results or solutions to prevent MDF. Attempts have been made to avoid MDF by improving the alignment between the SCL and sclera.14,18,20 Excessive clearance has not been found to be the primary cause of MDF 15,20, nor have care products, which appear to be the cause in only 27.0 % of cases.18
SCL wearers are also at higher risk of corneal infection due to extended contact with the saline.21 Contaminated solutions can lead to infection, as pathogens like Pseudomonas aeruginosa and Escherichia coli can survive in the solution for weeks, causing microbial keratitis.18
The purpose of this study is to collect and analyze practitioner data on filling solutions and demographic information. It also attempts to identify preferences and trends in the use of SCL filling solutions by surveying practitioners in German-speaking countries.
Material und Methods
The study followed a prospective, multivariate, cross-sectional design and was based on a time-limited empirical survey. It was conducted over a seven-week period (November 13 to December 31, 2023). The survey was written in German and created using the online tool Easy Feedback (Koblenz, Germany). A total of 24 structured questions covered three areas: general experience with SCLs, filling solutions, and individual approaches to SCLs including demographic information. The survey was distributed via an online link.
Professional networks and associations, including Falco-Linsen AG (Tägerwilen, Switzerland), Hecht Contactlinsen GmbH (Freiburg, Germany), and Interlens e. V. (Munich, Germany), distributed the link to contact lens practitioners across Germany, Austria, and Switzerland. Practitioners with experience in fitting SCLs were included, while those who do not fit SCLs were excluded.
This study analyzes qualitative and quantitative data from an exploratory survey using Microsoft Excel (Microsoft Corporation, Redmond, USA) and descriptive statistical methods. Bar and pie charts, as well as tables, illustrate frequency distributions, while boxplots visualize the median, dispersion, and range for a few questions. The goal was to identify trends and provide an overview of the data. Due to methodological limitations, no further statistical tests were conducted.
Results
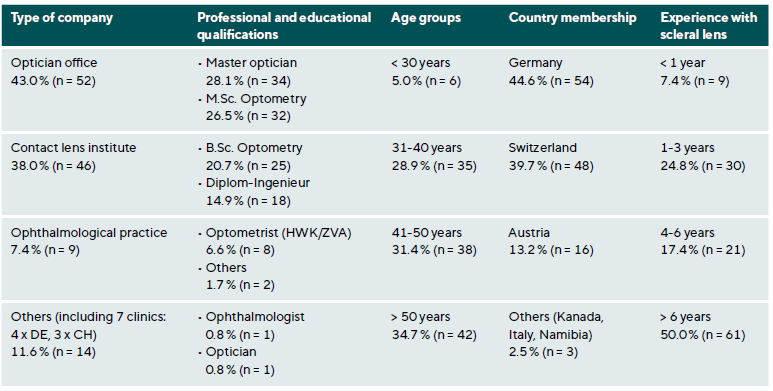
A total of 146 institutions responded, 121 of those provided complete datasets for statistical analysis. Table 1 presents an overview of the participants‘ demographics. A total of 50.4 % (n = 61) of participants have been fitting SCL for more than six years. The remaining 49.6 % are distributed across three groups: those with less than one year, one to three years, and four to six years of experience with SCL. The majority of the sample is employed in optician offices (n = 52) or contact lens institutes (n = 46) and the distribution between Swiss (n = 48) and German fitters (n = 54) is relatively even.
When asked whether scleral lenses are the preferred type of lens, the overall median (n = 121) was 2 (0 = strongly disagree, 10 = strongly agree). Experienced fitters (> 6 years) had a median of 3, while those with 1–3 years of experience had a median of 1.5.
Participants also indicated how often they fit scleral lenses for predefined indications. The most common indications were advanced keratoconus (62.0 %), post-keratoplasty (39.2 %), and irregular corneas (34.5 %). However, scleral lenses were less frequently used for OSDs (e. g., sicca syndrome, 28.6 %) or for mild to moderate keratoconus (16.8 %).
All respondents (n = 121) perceived the effort required to fit SCLs as relatively high, with a median score of 3 (0 = very high, 10 = very low). More experienced fitters rated the effort lower (4–6 years: median = 4; > 6 years: median = 3), while beginners (< 1 year) reported a median of 2.
They were also asked about the perceived difficulty of fitting SCL. On a scale of 0-10 (0 = very high, 10 = very low), the overall median was 4 (moderate-high). Beginners had a median of 2, those with 1-3 years of experience had a median of 3, and more experienced practitioners (4-6 years and > 6 years) had a median of 5.
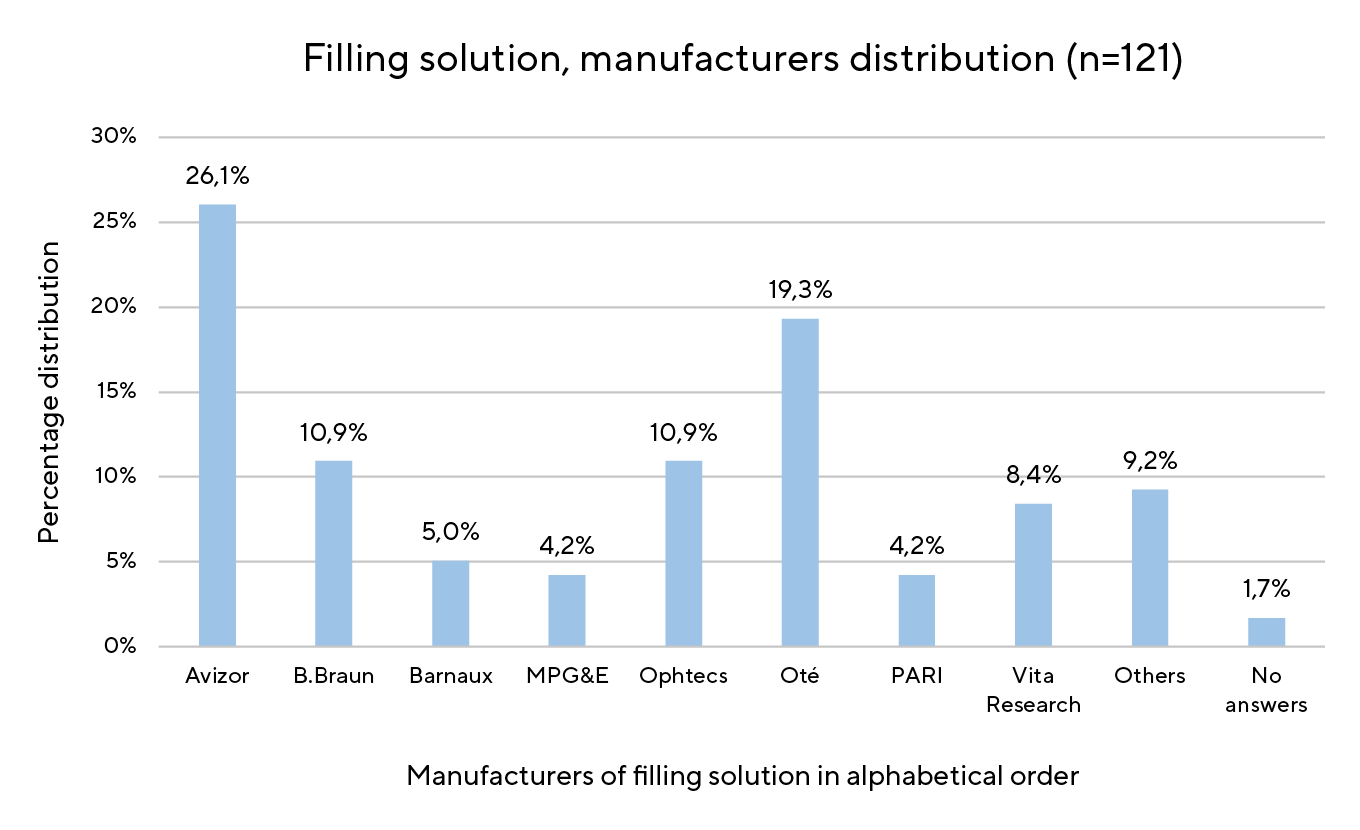
Figure 1 illustrates the percentage distribution of the eight most commonly cited filling solutions, with the ‚Others‘ category summarising manufacturers mentioned fewer than four times. The eight most frequently mentioned filling solutions were grouped into three catergories according to their ingredients which is shown in Table 2. Here the types of saline were listed with their components and their pH values, along with their associated products. In Figure 2, the percentage distribution of the whole sample size is shown, with the data presented in a range of columns.
Regarding the complete sample, Figure 2 demonstrated that 0.9 % NaCl without additives was the most commonly used product, favoured by a slight majority (35.5 %), followed by NaCl + B (30.6 %) and NaCl + E (19.0 %). In 13.2 % the solutions did not fit properly into one of the three categories.
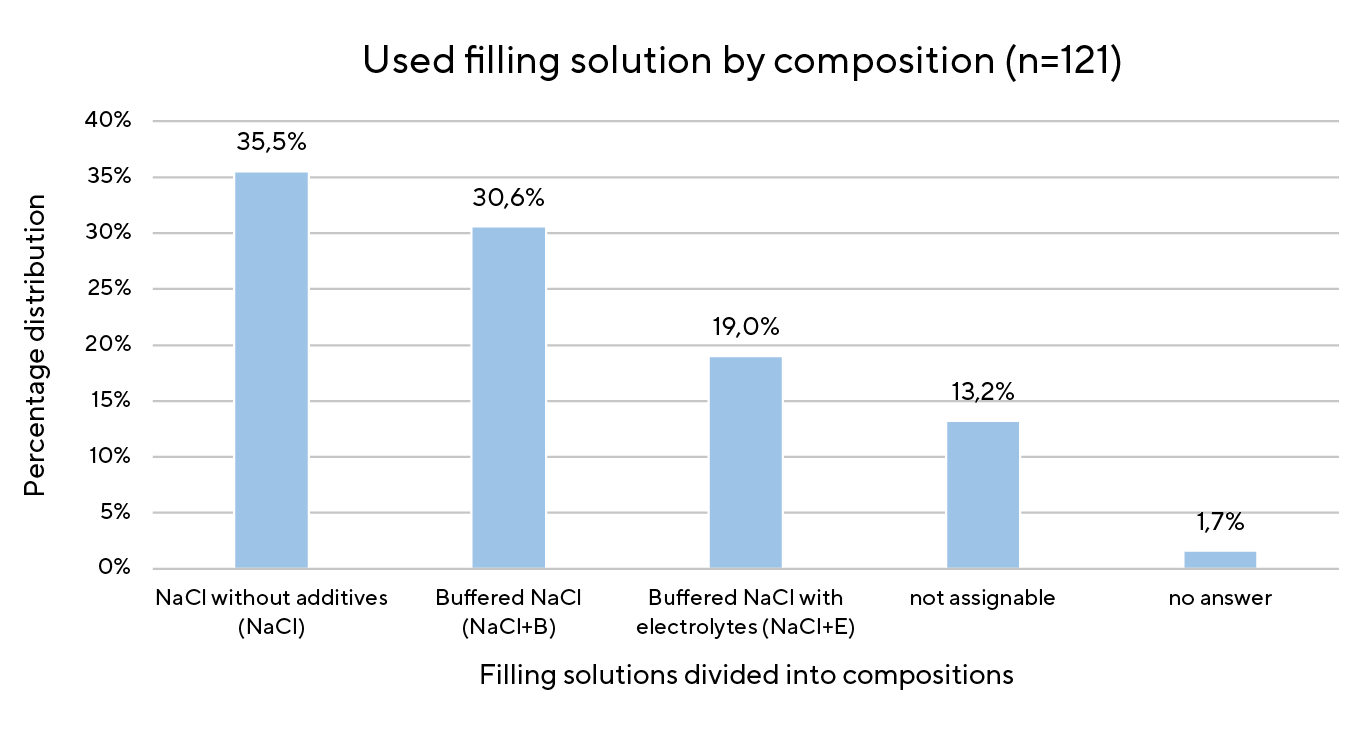
However, notable differences emerge when the country distribution percentages are considered across the product categories. This is shown in Figure 3 when the columns are split into the different countries (Germany = blue; Switzerland = red; Austria = grey). Only Swiss SCL practitioners use NaCl + E. NaCl without additives is the most often referenced in Germany while NaCl + B is the most common filling solution in Austria. The three additional countries (Canada, Italy, Namibia) were not included in Figure 3, as the figure focuses on the distribution within the German-speaking market.
When asked about the main reason for choosing a particular filling solution, most participants cited good patient tolerance (81.0 %) as the primary factor, followed by availability (45.5 %). Price played a minor role (9.1 %). Figure 4 shows the percentage distribution of responses; multiple answers were possible.
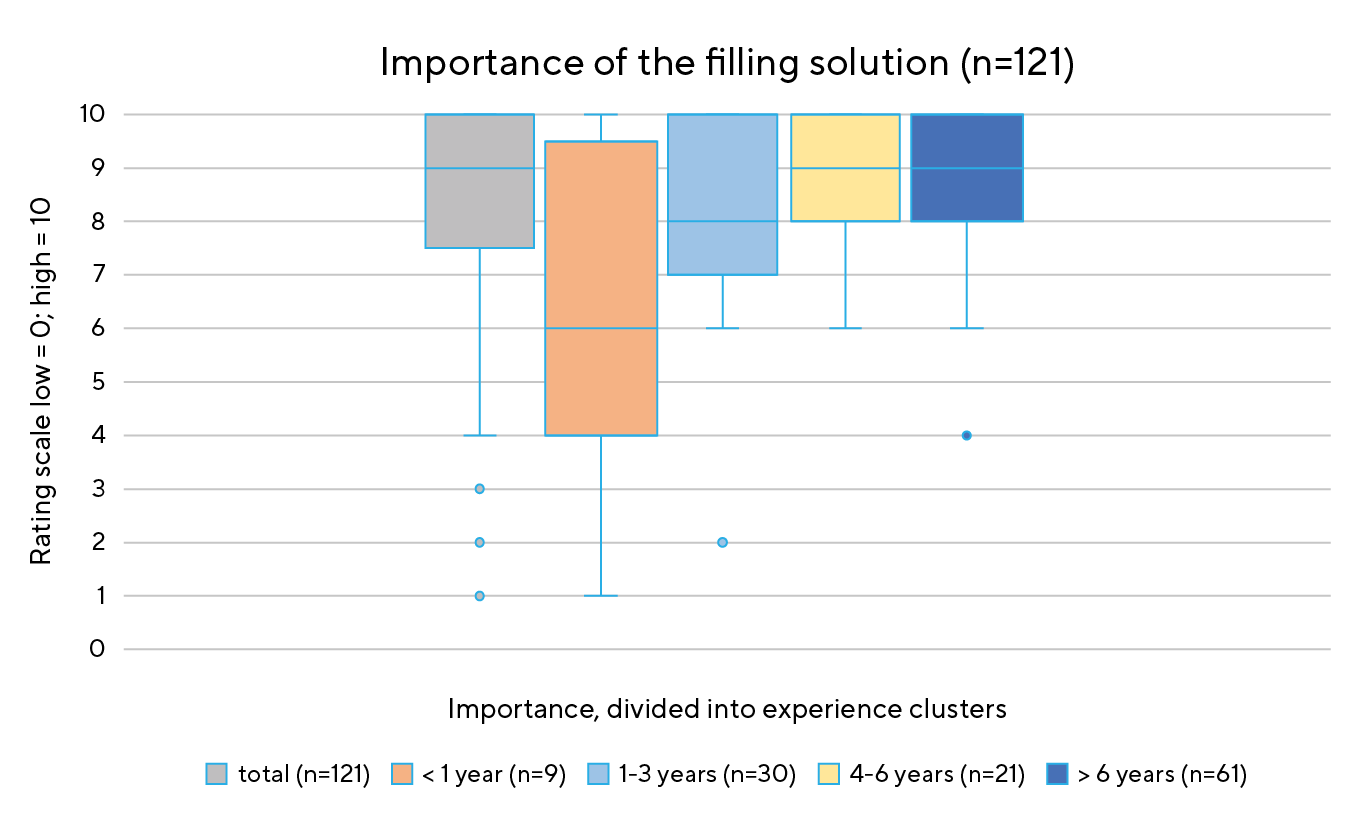
In a rating of the perceived importance of the filling solution, respondents (n = 121) assessed it as generally high to very high, with an overall median of 9 (0 = low, 10 = high). Beginners (< 1 year) considered it less important (median = 6), while more experienced practitioners (4–6 years and > 6 years) reported a median of 9. (Figure 5) Figure 6 illustrates the use of single-use vials for filling SCLs: the majority 73.6 % (n = 89) use sterile, non-preserved saline in single-use vials, 19.0 % (n = 23) did not reply, and 7.4 % (n = 9) reported larger container sizes.
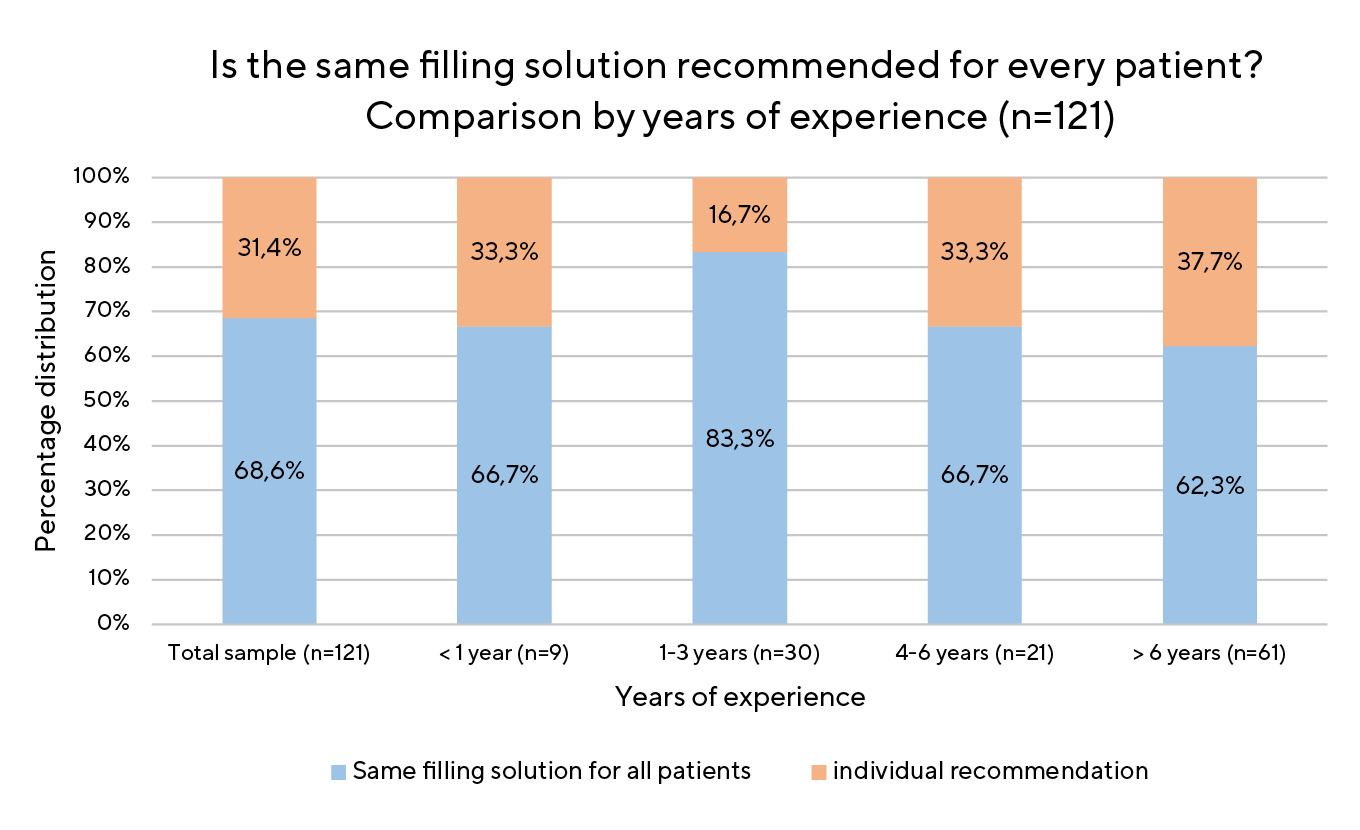
Participants were also asked whether the same solution is used for all SCL patients. Figure 7 shows the responses: 68.6 % (n = 83) agreed, while 31.4 % (n = 38) disagreed. Similar results emerged when the data were analysed by place of work or years of experience. Figure 7 also shows that experienced SCL practitioners select the filling solution slightly differently to those who have recently started fitting. Fitters with more than six years of experience (37.7 %) were more likely to recommend a customised filling solution than novices (33.3 %).
In addition to focusing on filling solution practices, other aspects relevant to the fitting process were explored, including the direct sale of filling solutions. Of the respondents, 87.6 % (n = 106) indicated that they sell the solution directly to their patients.
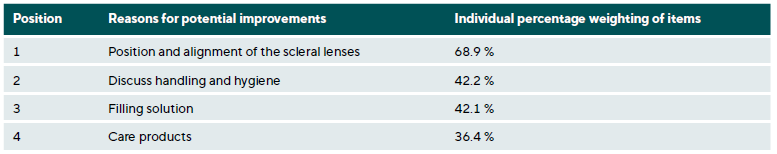
When asked about their approach to managing patient complaints, participants ranked a predefined fourstep trouble shooting sequence according to personal preference. Across the entire sample, the filling solution was most commonly placed in third position (Table 3), with second and third place appearing interchangeable. When the results were stratified by experience level, only minor variations in ranking patterns emerged.
Discussion
Detailed segmentation of experience into four groups (< 1 year, 1-3 years, 4-6 years, > 6 years) provides precise insights into the professional development of practitioners. The findings indicate that the propensity to fit SCL increases with experience. With regard to the most common indications for SCL – advanced ectasia, post-keratoplasty, and irregular corneas – the results are consistent with those of the study by Shorter et al.22 In that study, SCL were also frequently the first choice for irregular corneas but tended to be one of the last options for OSD.
Furthermore, the results show that both the effort required and the perceived difficulty of fitting SCL decrease with increased experience. A study by Schornack et al. confirms this trend, demonstrating that experienced practitioners require fewer appointments to successfully fit SCL.23
The recommendation to use sterile, preservative-free saline in single-use vials was followed by 73.6 % of participants (Figure 6), which is in line with the findings of Schornack et al.3,24
Additional buffers (borate, phosphate) provide pH value stability and isohydration, reducing or eliminating irritation of the anterior segment.8,13 This property benefits all solutions that come into direct contact with the anterior eye or tear film, such as contact lens care products, artificial tears, and ophthalmic drugs.
According to the Federal Institute for Drugs and Medical Devices (BfArM), buffer solutions are classified as excipients 25,26 and therefore, neither the exact ingredients nor their concentration needs to be specified.26,27 While buffer substances have been shown to have negative effects on human corneal-limbal epithelial (HCLE) and human conjunctival epithelial cells (HCjE) 13,25, no adverse effects are observed at very low concentrations.28 The exact formulas of buffered salines remain unknown.11,12
Further evidence for the physiological importance of solution composition comes from an experimental study by Bergmanson et al., who compared the effect of NaCl and glutathione bicarbonate Ringer’s (GBR) solution on rabbit corneas. Corneas exposed to NaCl alone showed significantly more epithelial damage—characterised by abnormal and sloughing cells—than those bathed in GBR, indicating that NaCl alone is insufficient to maintain epithelial integrity.29
Only a few studies have investigated the use of different filling solutions for SCL wearers. Montanti demonstrated that objective quality of vision (OQV) remained unchanged for hours with NaCl + E (Isosol, Vita Research) in MDF affected SCL wearers, whereas OQV decreased with NaCl + B (Soluzione Salina, Alcon).16 Fogt et al. showed that the OSDI score and subjective irritation decreased in MDF patients when using individual filling solution with electrolytes (pH 7.2-7.6), compared to the NaCl control saline (pH 4.5-7.0).17 Tse et al. concluded that for healthy corneas, the type of saline used does not significantly matter. They compared NaCl (Addipak, Teleflex Medical pH ~5.3) with NaCl + B (Purilens Plus, Life-style Company Inc., borate buffered, pH ~7.5).30
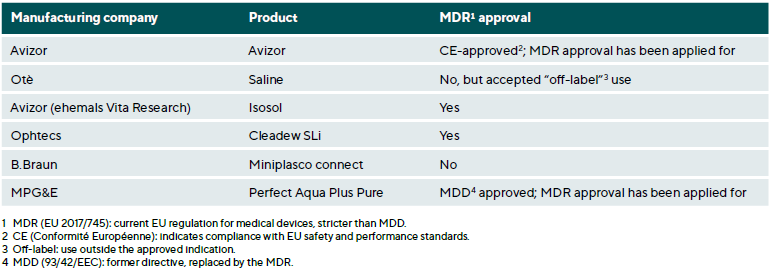
As part of this study, the five main suppliers of filling solutions were contacted. They were asked whether their respective product is approved for the intended use as a filling solution for scleral lenses. While some of the products are officially approved for this specific use, others are used off-label. The responses are summarised in Table 4.
However, there are no guidelines regarding whether the lens should be filled with isotonic saline (NaCl), buffered saline (NaCl + B), or electrolyte-enriched saline with viscosifying additives (NaCl + E).
Conclusion
This study provides detailed insights into the practice of SCL fitting, focusing on the use and distribution of filling solutions in German-speaking countries. The survey reveals that while most practitioners are satisfied with their saline solutions, notable differences in preferences between countries exist. German respondents favor isotonic saline (NaCl), while Swiss practitioners prefer buffered, electrolyte-enriched saline (NaCl + E). Austrian participants tend to use borate-buffered saline (NaCl + B). Despite these differences, most fitters use preservative-free single-use vials to minimize the risk of infections.
A common issue in SCL use is MDF. This occurs when protein, lipid, and cell deposits accumulate in the fluid reservoir, causing it to become cloudy and impairing the patient’s vision. While electrolyte-enriched saline has been shown to improve comfort and potentially reduce MDF, the problem remains largely unresolved.
The survey concludes that all three types of filling solutions (NaCl, NaCl + B, and NaCl + E) are recommended by practitioners and well-tolerated by patients. In cases where a solution does not meet expectations, alternatives are available. Delayed market introduction or low awareness may explain the limited use of NaCl + E solutions in Germany and Austria. The survey demonstrates the importance of ongoing research to determine the optimal filling solution for different patient groups, with a focus on improving comfort, vision quality, and eye health.
Funding
This research did not receive any specific grant from funding agencies in the public, commercial, or not-for-profit sectors.
Conflict of interest
The authors declare that they have no known competing financial interests or personal relationships that could have appeared to influence the work in this paper.
Cells. Cornea, 36, 712–718.
Referencing: 07 August 2024.