The feasibility and tolerability of bright light therapy in childhood myopia: A pilot study
Purpose: This study aims to investigate the feasibility and tolerability of morning bright light therapy (BLT) in children with myopia. Additionally, any potential benefits of morning BLT in reducing myopia progression will be explored.
Material and Methods: This was a pilot study exploring the tolerability and feasibility of BLT. A total of 15 children (7 - 13 years) attended two visits, 6 months apart in either the BLT group, myopia management spectacles or contact lenses and BLT (BLT-MMI) group or the control group. Questionnaires
collected data on tolerability and feasibility of BLT. A weekly paper diary on compliance was completed. Ocular measures included axial length, vitreous chamber depth, spherical equivalent refraction (SER) and subfoveal choroidal thickness.
Results: Children were, on average, 9 years old (SD 1.6 years), baseline SER −1.86 D (0.62 D), baseline axial length 24.67 mm (0.83 mm), 53.3 % female and 53.3 % white. BLT (control n = 4, BLT n = 4, BLT-MMI n = 7) was used on average 84 % (SD 12 %) of the time with compliance poorest over school holidays. There was one report of occasional eyestrain, 91 % of parents reported BLT was easy to use routinely and 91 % of children were happy to use BLT. There was no difference in the change in ocular measures between groups (all p ≥ 0.07).
Conclusion: BLT provides a tolerable and feasible intervention with good compliance. Future research should consider closer monitoring of compliance over the school holidays. The current analyses were limited by the small sample size and therefore research is required to explore the efficacy of BLT
in myopic children both as a standalone and a combination therapy.
Background
The World Health Organization (WHO) considers uncorrected refractive error due to myopia (short-sightedness) to be one of the major causes of visual impairment.1 The prevalence of myopia has increased across the world, most considerably in East Asia 2 but also in the UK 3 where the prevalence is 18.6 % by 17 years old in Northern Ireland 3 and 29.4 % by 12-13 years old in Birmingham, England.4 Myopia primarily arises during childhood from excessive elongation of the eyeball which progresses for most until their late teenage years.5,6 In uncorrected myopia, the image is focussed in front of the retina, resulting in blurred distance vision requiring spectacles or contact lenses to correct vision. The increased axial length may increase the risk of sight threatening pathologies such as retinal detachment which may lead to visual impairment particularly in those with high myopia.7,8 Visual impairment is associated with depression,9 and vison related quality of life.10 Myopia can have major lifelong implications and, in children, poor vision and uncorrected refractive error negatively affects academic performance, attention 11 and reading performance.12
Myopia is multifactorial with less time spent outdoors, greater time spent on near work and parental myopia being the most notable risk factors for the onset of myopia.13 Additionally, within Scotland, the proportion of children wearing glasses for myopia varies by socioeconomic status with a trend towards more myopia in more deprived areas.14 Within the UK, the climate varies considerably by season and region and these climatic challenges are likely to influence how often a child can spend time outdoors. In particular, more northern parts of the UK, such as Scotland, experiences a wetter climate and has fewer hours of sunshine than England (Annual hours of sunshine: Scotland = 1238.9 hrs, Eng-land = 1675.4 hrs).15 This may mean spending more time outdoors is difficult for children living in locations such as these.
Myopia management interventions (MMI) include specialised contact lenses and spectacle lenses 16 which are available in the UK to slow the progression of myopia in children. Whilst treatments exhibit a similar efficacy on average, there is variability in intervention success within a clinic population.17,18 Additionally, it is not possible to identify which child is most likely to benefit from an intervention. MMIs can be costly and are required until myopia normally stabilises in late teenage years.5,6 Light therapies have recently emerged as a potential MMI and also as a potential additional therapy for children not responding as expected to MMI. Light therapies to date include red light therapy, bright light therapy (BLT) and blue and violet light therapy. A systematic review and meta analysis reported that red light therapycan slow the progression of myopia in children.19 The mechanism is not fully understood but theories include that it may stimulate the mitochondria within the cells responsible for energy production, promoting a decrease in retinal inflammation.19 Other theories include it may stimulate an increase in choroidal blood flow, reducing oxidative stress and inflammation.20 The choroid is a vascular layer located between Bruch’s membrane and the sclera. It demonstrates dynamic changes in response to the optical environment and pharmacological interventions by thickening or thinning.13 Other evidence indicates that the choroid may help regulate biochemicals influencing myopic growth via growth factors.21,22 However, there have been some concerns on the long term safety of some red light therapy devices.23 Additionally, red light therapy ($ 11,478 over a five year period 24 is considerably more expensive than other light therapies such as BLT (£ 99 per lamp 25).
Research has also explored the potential for blue light therapy in adults 26, through stimulation of the blind spot, and found an increase in choroidal thickness and also through the use of glasses emitting blue/green light.27 Violet light therapy has also been considered in a recent pilot trial 28 but effects were modest in the cohort overall.28,29 Once again, the mechanism is unclear but is thought to involve modulation of choroidal thickness through stimulation of retinal photoreceptors.
BLT may provide a more affordable, safe and natural intervention whilst providing an alternative to spending time outdoors during inclement climate and during the darker months of winter in the UK. BLT includes the use of lamps designed for Seasonal Affective Disorder, which mimic natural daylight and are typically used for 20 - 30 minutes in the morning. These lamps have been found to be tolerated and safe to use, with few minor side effects including headache and eyestrain 30,31, particularly in otherwise healthy participants.32 Such lamps also contain UV filters meaning there is no significant risk of UV damage to the eyes or skin.33 Phototherapies are already used in the treatment of various paediatric disorders including jaundice,34 eczema 35 and Seasonal Affective Disorder (SAD).36
Research is yet to explore the potential for BLT in slowing myopia progression in humans. As with other light therapies, the mechanism is not fully understood and may involve modulation of choroidal thickness or entrainment of circadian rhythm (internal body clock) which has been previously implicated in myopic growth.37 To date, research is yet to explore the feasibility, tolerability and potential benefits of BLT in reducing myopia progression in children in the UK.
This study aims to investigate the feasibility and tolerability of morning BLT in children with myopia. Additionally, any potential benefits of morning BLT in reducing myopia progression will be explored.
Inclusion and exclusion criteria
Healthy children aged 7 - 13 years old were invited to participate. Children with reduced visual acuity, significant ocular comorbidities or binocular vision abnormalities, myopia of more than −10 DS or astigmatism of more than 4 DC were excluded from recruitment.
Materials and Methods
The study was advertised to optometry practices across the Central Belt of Scotland and advertised to parents via social media and advertisements. The study aimed to allocate a 1 : 1 ratio of BLT: control with the control group not using any MMI and wearing single vision spectacles only. Participants were randomised using minimisation to reduce any imbalance in factors 38 including age and refractive error
Participants were randomly allocated to either the BLT or the control group. However, due to the recent commercial availability of MMI within community optometry practices, many parents and children expressing interest in the study had already started using MMI. Therefore, any children who were already wearing MMI and who had expressed an interest in the study were also recruited to the study. These children were allocated to a third group which used BLT in addition to continuation of their own MMI (BLT-MMI group). These children had been prescribed MM spectacles or contact lenses by their community optometrist. These included peripheral defocus modifying spectacles or dual focus contact lenses. As a result, there were three groups: 1) BLT, 2) control and 3) BLT-MMI group. A fourth group wearing MMI only was not recruited as robust data are readily available on the efficacy and tolerability of these interventions 16 and the study aimed to focus on the tolerability and feasibility of BLT rather than MMI.
Children were seen at two visits at Glasgow Caledonian University separated by 6 months. The researcher was a qualified optometrist with experience in paediatric eye examinations and myopia management. Children were recruited between September 2023 and March 2024. Data collection took place between September 2023 and September 2024.
Intervention
The ‘Vitamin L’ lamp (Lumie®)25 utilised in the study is a class II a medical device, certified to UK MDR 2002 and EU MDR 2017/745. It is a lightweight portable lamp requiring a mains connection. The cool white, UV free LED bulb has a light intensity of 10,000 lux when placed at 20 cm which is similar to ambient daylight. These lamps were issued to children in the intervention groups (BLT group and BLT-MMI group) with instructions to use these lamps every morning until their follow up visit six months later. Lamps were to be positioned at 20 cm from the eyes and used for 30 minutes each morning. The lamp could be placed to the side of the child, allowing them to continue with an activity such as watching the TV or reading. A 20 cm ribbon was provided to parents to ensure a consistent distance was maintained. The child could continue to complete their normal activity such as reading or watching the TV during this 30 minute period.
Refraction and biometry
Refractive error was measured using cycloplegic autorefraction (Nidek ARK 500a) and spherical equivalent refraction (SER) determined as sphere+ (cylinder x 0.5) in each eye. Autorefraction was measured 30 minutes after the instillation of one drop of 1 % cyclopentolate. To determine if full cycloplegia had occurred, the amplitude of accommodation was measured. If the amplitude of accommodation was greater than 2 D, an additional drop of cyclopentolate was instilled and the amplitude of accommodation assessed again 30 minutes later until levels dropped below 2 D. A total of 3 measures were taken and the average used in analysis.
Axial length and vitreous chamber depth were measured using the Lenstar Myopia LS900. A total of five measures were collected from each eye for each and the average calculated for each. Corneal curvature was measured and the average of the two meridians reported.
Compliance and feasibility
Parents and children completed a paper diary documenting their usage of BLT. Parents reported whether the lamp was used each day and for how long. If a child used BLT for less than 15 minutes, this was counted as a ‘missed’ day. The percentage of days the lamp was used was then determined. Regular ‘check ins’ with parents and children were completed where they were reminded to complete the compliance log, to send photos of the compliance log and to report any issues surrounding the use of BLT, which were then discussed. These were completed weekly.
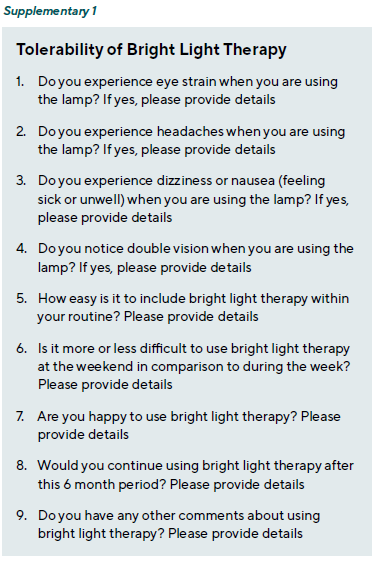
A mixture of open and closed questions was used to ask the parent and child about the tolerability and usability of the SAD lamp with specific questions relating to headaches, dizziness or nasuea or eyestrain (Supplementary 1). Parents and children were asked to comment on the ease of which BLT was included in their routine, the ease of using BLT at weekends, if they would continue using BLT after the study period and if there were any other comments about using BLT (Supplementary 1).
Demographic information
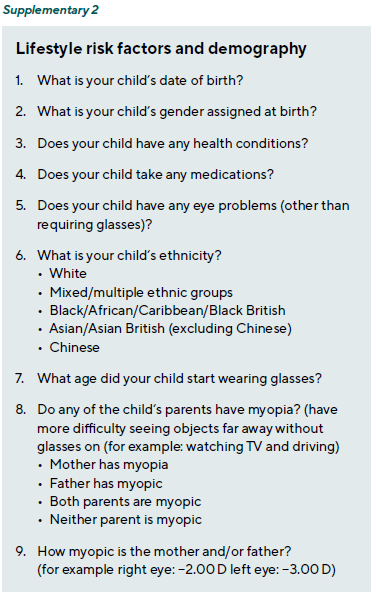
Data on the number of myopic parents and the severity of parental myopia based on selfreported refractive error (using SER: low = −0.50 to −2.99 D, moderate −3.00 to −5.99 and high ≤ −6.00 D) were gathered. Demographical information including ethnicity and gender was also collected (Supplementary 2).
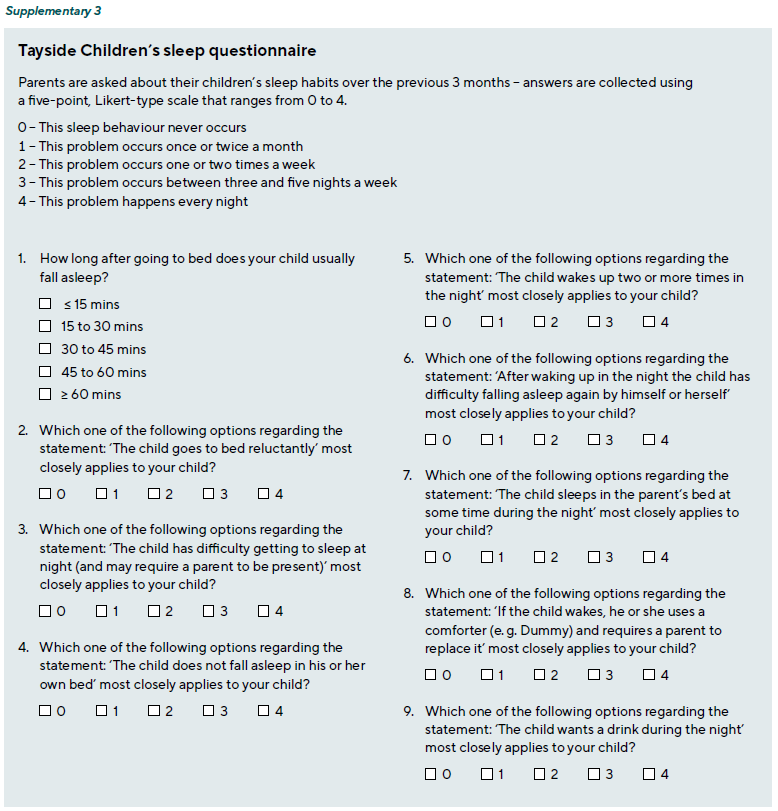
Data on sleep quality were collected using Tayside Children’s sleep questionnaire 39 (Supplementary 3) to determine any effects of the use of BLT on sleep.
Choroidal image analysis
All images were captured using the Topcon Triton OCTA. For each participant, a 6 mm macula radial scan was captured using the Fundus Guided Acquisition software to ensure OCT images were captured at the same location at each visit. Sub foveal choroidal thickness was analysed. Additionally, choroidal thickness 1.5 mm from the fovea measured superiorly, inferiorly, nasally and temporally was analysed at each visit. OCT B-scans were then processed with Choroidalyzer,40 a deep learning-based, fullyautomatic tool for analysis of the choroid. Choroidalyzer automatically segmented the choroid in each B-scan and measured choroidal thickness in five locations: subfoveally, and 1.5 mm from the fovea superiorly, inferiorly, nasally and temporally. For the subfoveal thickness, values were averaged across all radial scans.
Bias
All ocular measures are objective and therefore reduce the risk of bias. However, it was not possible to mask the research-er or the parent and child to the intervention type. Choroidal image analysis was performed by JE who was masked to the treatment type.
Patient and Public Involvement
Patient and public involvement interviews were conducted to evaluate aspects of the study design including duration of study visits, recruitment strategies, methods of monitoring compliance and study result dissemination.
Ethics
The study was registered with ISRCTN (ISRCTN25433872). Informed consent was obtained from parents and informed assent obtained from children prior to any measures. Ethical approval was granted from the Health and Life Sciences Ethics committee at Glasgow Caledonian University (HLS/LS/A22/074). This research was conducted in accordance with the declaration of Helsinki.
Statistical analysis
Due to a high level of correlation between right and left axial length (r = 0.90, p < 0.001), data from the right eye are pre-sented as commonly reported within vision research.41 One-way ANOVA was used to analyse differences in continuous variables by categorical variable. Fisher’s exact test was used to evaluate differences in categorical variables.
Data analyses were performed using Stata 13.1 (Stat-aCorp Texas, USA) using a statistical significance level of 5 % (p < 0.05).
Results
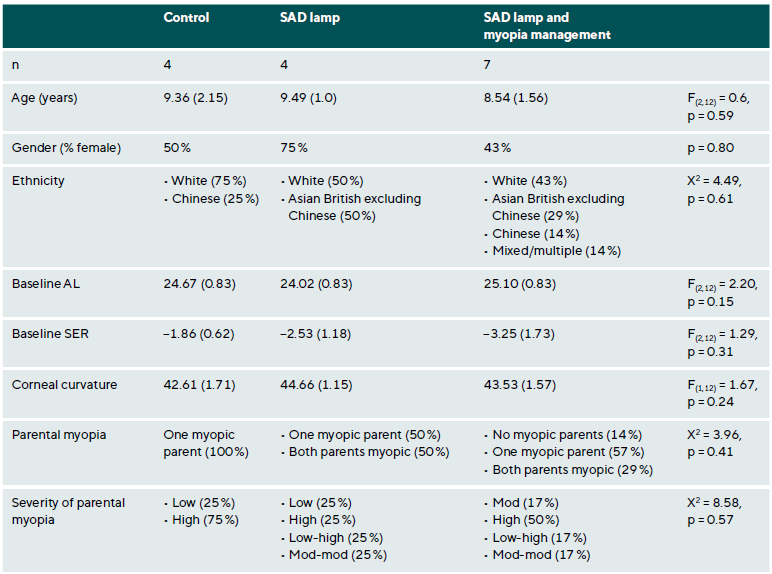
Baseline characteristics
A total of 15 children (mean age 9 years, SD 1.6 years) were recruited with 4 children recruited to the control group, 4 children recruited to the BLT group and 7 children recruited to the BLT-MMI group. There were no drop-outs over the study period and all children who attended for screening were eligible for recruitment. The characteristics of the children by group are described in Table 1. There was no significant difference in characteristics by group (all p > 0.15).
Compliance and feasibility
All children and parents preferred to use BLT at home before starting school. Compliance was documented by parents and children using a diary. The majority of parents and chil-dren returned completed paper diaries (n = 14). One parent opted for an electronic diary but failed to complete the di-ary. Compliance ranged from 63 to 97 %, average of 84 % (SD 12 %). Inspection of paper diaries showed that times of poor compliance occurred when parents and children were away on holidays.
BLT was well tolerated with no children reporting headaches, dizziness or diplopia. There was one minor adverse event with one report of occasional eyestrain due to brightness of the lamp which did not affect compliance or use of the lamp. One child reported:
‘it was very bright to start with but got used to it’ – Child 11 Of those using BLT, a total of 91 % (n = 10) of parents re-ported that it was easy to incorporate into their routine and 91 % reported that they will continue using the lamp after the research study. Particularly, parents reported the ease of using BLT in their morning routine:
‘Using the lamp structured the morning routine better’ –Parent 8
‘very easy to use, they sat by the chair and used their ipad or watched tv’ – Parent 12
A total of 91 % of children reported they were happy using BLT although one child reported:
‘It is sometimes annoying remembering to do it’ – Child 10 One parent reported:
‘As days got lighter, less inclined to use. They struggled with sitting still for 30 mins’ – Parent 11
Parents also commented on the ease of portability of the lamp as it is lightweight and easy to transport. A total of five parents reported that BLT was not any more difficult to use over the weekend, one parent reported it was easier to use at the weekend whilst five parents reported it was more difficult to use over the weekend.
Parents reported during the appointment visit that they had not observed any change to their child’s mood or sleeping pattern following initiation of BLT. However, when sleep scores were analysed, there was a significant improvement in sleep score at baseline (IQR 4 (1.5 - 8)) in comparison to sleep score at 6 months (3 (1 - 5)) (p = 0.05). Sleep scores above eight indicate difficulties initiating or maintaining sleep.39 At baseline, there were three children with a sleep score greater than eight (scores of: 11 (child 1),13.5 (child 2) and 20 (child 3)) indicating abnormal sleep patterns. Two of these children demonstrated a shift towards normal sleep score (scores of: 4 (child 1) and 3 (child 3) over the 6-month study period with the remaining child demonstrating no change (13, child 2).
Regarding protocol deviations, two children refused the use of cyclopentolate eye drops at all visits with one child being in the control group and the other child in the BLT-MMI group. At baseline, the measurement of AL and VCD could not be completed on two of the children (one within the control group and one within the BLT-MMI group). There were no other protocol deviations.
Change in myopia progression
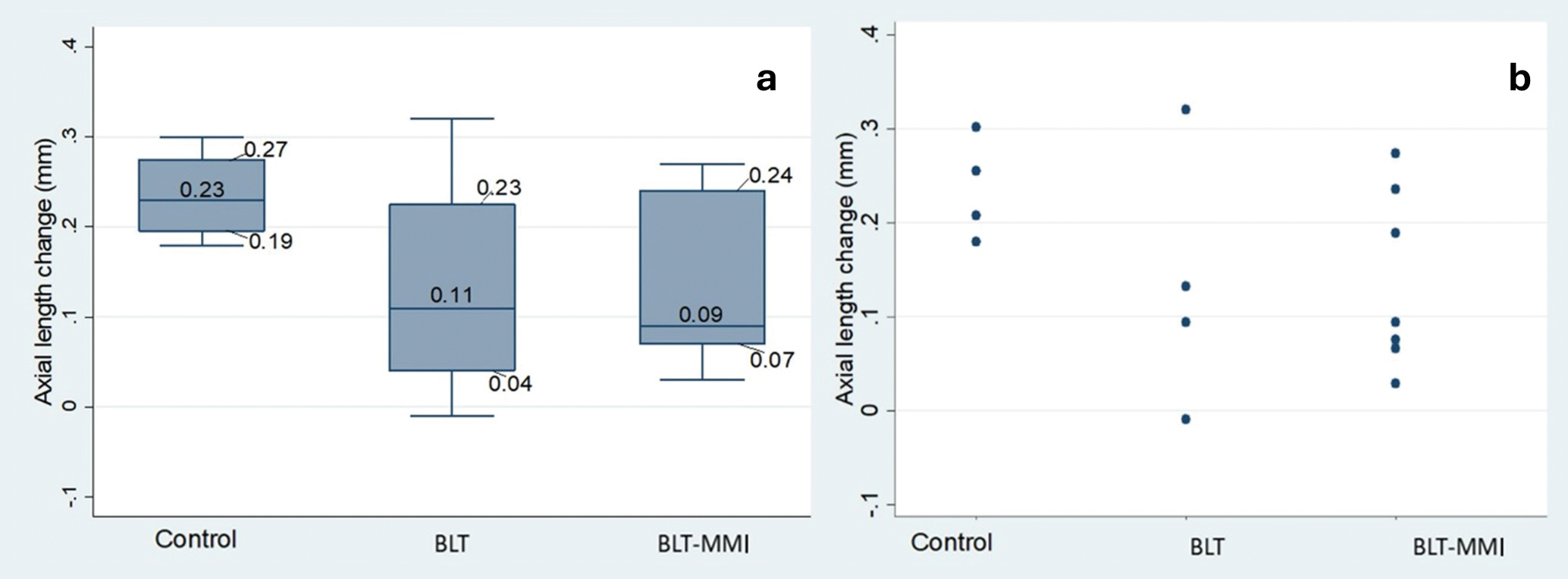
Although there was a trend towards less axial elongation in the BLT group (median change 0.11 mm (IQR 0.04 - 0.23 mm) and the BLT-MMI group (0.09 mm (IQR 0.07 - 0.24 mm)) in comparison to the control group (median change 0.23 mm (IQR 0.19 - 0.27 mm)), there was no statistically significant difference between groups (F(2,12) = 1.46), p = 0.29) (Figure 1).
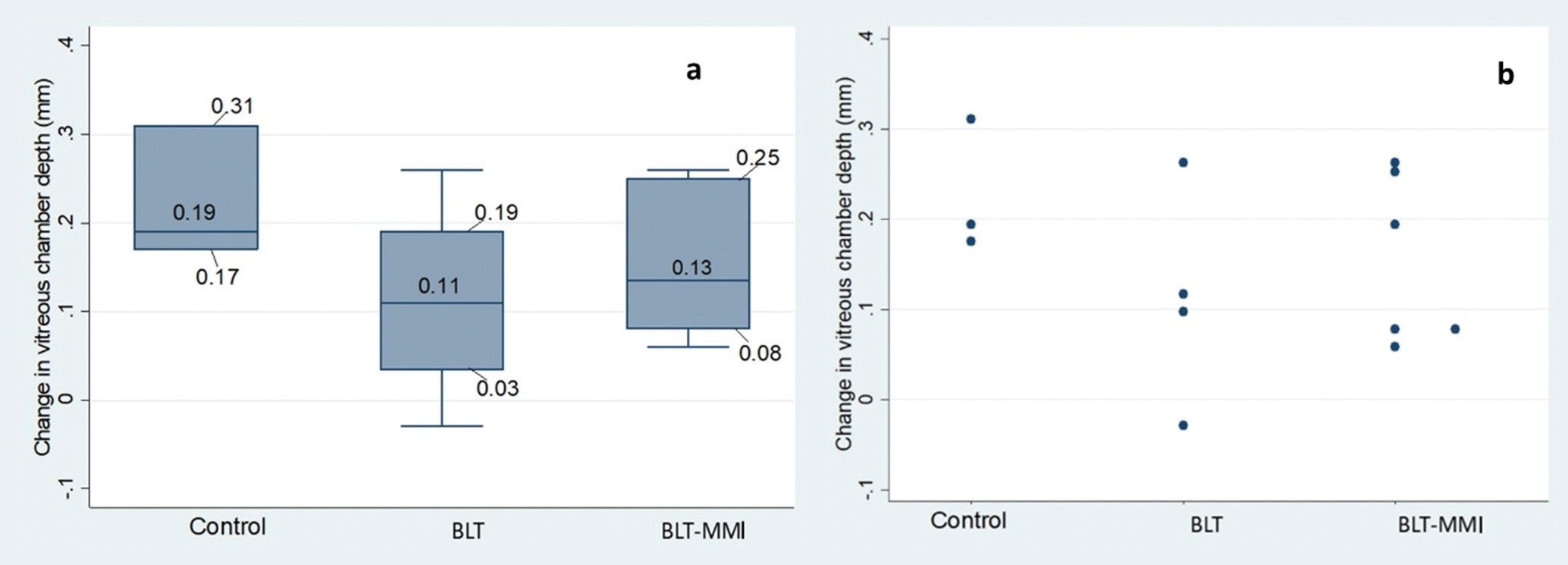
There was a trend towards less vitreous chamber deepening in the BLT group (median change 0.11 mm (IQR 0.03 - 0.19 mm)) and the BLT-MMI group (0.13 mm (IQR 0.08 - 0.25 mm)) in comparison to the control group (medi-an change 0.19 mm (IQR 0.17 - 0.31 mm)) but the difference between groups was not statistically different (F(2,12) = 1.11), p = 0.37) (Figure 2).
Spherical Equivalent Refraction (SER)
There was no significant difference in SER progression between the BLT group (median −0.19 D IQR −0.37 to +0.56 D), the BLT-MMI group (median −0.38 IQR −0.88 to +0) and the control group (median −0.41 D IQR −0.89 to −0.16 D) (F(2,12) = 0.95, p = 0.42) (Figure 3).

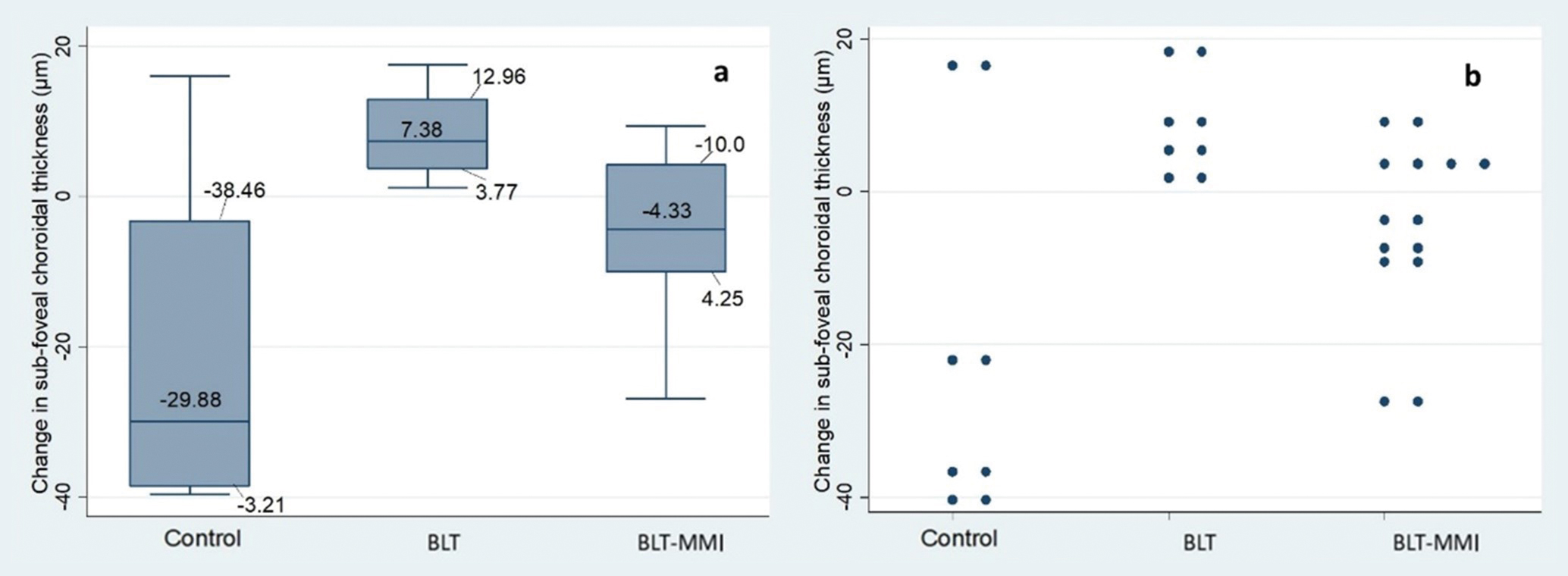
Change in choroidal thickness
Sub foveal choroidal thinning occurred in the control group (median −29.88 µm IQR −3.21 to −38.46 µm) and the BLT-MMI group (median −4.33 µm (IQR 4.25 to −10.0 µm) whilst choroidal thickening occurred in the BLT group (median 7.38 µm IQR (3.77 to 12.96 µm) (Figure 4). There was no statistically significant difference in the choroidal thickness response between groups (F(2,12) = 3.45, p = 0.07).
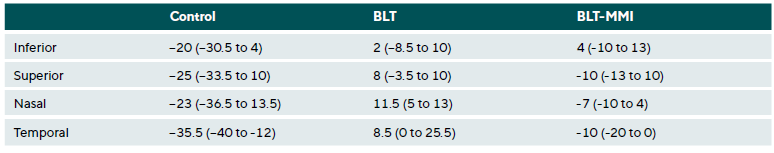
When choroidal thickness was analysed by location (superior, inferior, nasal and temporal), there was no difference in choroidal thickness by location within the control group (F(3,12) = 0.28, p = 0.84), the BLT group (F(3,12) = 0.67, p = 0.59) or the BLT-MMI group (F(3,24) = 0.96, p = 0.43).
There was no significant difference between intervention groups when considering the amount of change in superior choroidal thickness (F(2,12) = 3.63, p = 0.06), inferior choroidal thickness (F(2,12) = 0.82, p = 0.47) or in nasal choroidal thickness (F(2, 12) = 1.22, p = 0.33) (Table 2). The change in temporal cho-roidal thickness was significantly different between groups (F(2,12) = 3.75, p = 0.05) with the control group demonstrating greatest choroidal thinning followed by the BLT-MMI group whilst the BLT group demonstrated choroidal thickening (Table 2).
Discussion
This is the first study to the authors’ knowledge which has explored the use of BLT in children with myopia in the UK. The data from this study suggests that BLT may be a tolerable and feasible intervention for myopia. Further work using a larger sample size over a longer period of time is warranted to further confirm the effects of these lamps on eye growth and choroid thickness changes in slowing the worsening of childhood myopia. This is of particular note as this pilot study is limited in the conclusions that can be determined from the small sample size.
BLT was well tolerated with just one child reporting minor eyestrain which did not affect compliance or usage of the lamp. This agrees with a recent review paper finding that the use of seasonal affective disorder lamps in adolescents is well tolerated with few adverse effects.30 This is the first time that tolerability of BLT in myopic children has been explored. The majority of parents reported that BLT was easy to incorporate into their routine and that they would tend to use it after the study finished. Results suggested that it may be more difficult for parents and children to use BLT over the weekend, during school holidays and in the brighter months and therefore future research should consider issuing reminders on compliance coming up to the weekend and consider closer monitoring over the brighter months and holiday periods.
Although there was a clinically meaningful slowing in axial elongation (0.1 mm / 6 months) following BLT, which is similar to the equivalent slowing in myopia progression observed in children using specialised spectacles or contact lenses (on average 0.1 / 6 months) 42,43,44, this was not statistically significant. This is likely due to the sample size with power calculations (significance of 0.05, power of 90 %) indicating that 25 children in each group would be required to detect a statistically significant difference of 0.1 mm. This further highlights that the small sample size limits the conclusions that can be made about the potential benefits of BLT on myopic progression.
BLT may be used in addition to myopia management spectacles or contact lenses and may provide an additive therapy. However, results from this study did not confirm an additive effect, this may be due to variability in treatment effects when using myopia management spectacles 17 or it may be that the small sample size is not representative of a larger population and that the analysis was not sufficiently powered. Further research is required to confirm this. Despite this, this study may help form the basis for future studies exploring the use of BLT as a single therapy as well as an additive therapy.
MMIs have recently become commercially available in the UK to community optometry practices. This has resulted in challenges surrounding recruitment due to many children now already using MMI. Recruitment approaches in this study were extensive and included social media advertisement, talks delivered to practitioners to encourage referrals, dis-tribution of study information in schools, after school clubs and optometry practices and referrals from practitioners.
Discussions with parents and observations from the research assistant confirmed that referrals from practitioners and media advertisement were most likely to be effective for recruitment. This has provided useful insight into new and future challenges facing myopia research. In particular, future studies in the UK may wish to consider the use of future ‘virtual’ control groups 45 or cross over design trials 46 as a more ethical and cos-effective option and to mitigate recruitment issues surrounding a control group.
There was a trend towards less choroidal thinning in the BLT group which has also previously been reported in adults.36 The difference in subfoveal choroidal thickness changes in this study in the BLT group (mean increase of +8.36 µm) is sim-ilar to that reported by Read et al. 2018 36 (mean increase of +5.4 µm) in adults. Studies have yet to reported on differential changes in choroidal thickness by location in response to BLT. This study found that choroidal thickness changes did not vary by location. When comparing between locations, temporal choroidal thickness changes varied significantly. Due to the variability within the data, these findings should be replicated in a large sample size to evaluate if there are localised differences in how the choroid changes in response to BLT.
Further research should continue to explore non-optical based interventions for myopia in a bid to determine a more affordable method of slowing myopia progression. MMI is largely privately paid for by the parent. Cost effectiveness research to date in the UK has indicated that MMI options including specialised spectacles may not be cost effective in comparison to reusable contact lenses including ortho-keratology.47 However, the report included data from MMI which have not been effective in slowing progression and, at the time, data on long term effectiveness were not available. BLT may provide a more cost-effective intervention and this study provides preliminary data suggesting that further research is required to explore the efficacy of what could be a well-tolerated and feasible intervention.
There was a statistically significant improvement in sleep scores between visits. This would suggest an improvement in sleep quality which has also been reported following BLT in those with depression 48 and in the elderly.49 Other research also reports an improvement to mood and reduction in day-time fatigue.50 However, much of the research to date has been conducted in adults or adolescents with conditions such as depression 48,51, insomnia 50 or cancer.52 Previous research has not explored this topic in otherwise healthy children.
However, the small difference in sleep score noted in this study is unlikely to be clinically meaningful. Sleep scores above eight indicate difficulties initiating or maintaining sleep.39 There were three children with a sleep score greater than eight indicating abnormal sleep patterns. Two of these children demonstrated a shift towards normal sleep patterns (score of less than eight at six months) and the remaining child demonstrated no change. However, this is unlikely to be attributed to BLT as only one child utilised a lamp which may indicate that variations in sleep patterns may have occurred due to other reasons such as the home environment.53
Limitations
A main limitation of this study is the small sample size. As a result, data may not be representative of the population as a whole and statistical analysis were likely underpowered. Another factor that should be considered a limitation is that data on the intensity of the room illumination the child was sitting when using BLT was not collected. Therefore, it’s unknown if the intensity of the room lighting may have affected tolerability or the effects of BLT on eye growth. Regardless, the small sample size limits any conclusions that can be made on the effects of BLT on eye growth. Compliance was documented using paper diaries by the children with regular check ins from the research team. The BLT used in this study did not have a built-in option to monitor compliance. Despite this, completion rate was high indicating that at least over 6 months, paper diaries may be used to document compliance when using BLT. A total of two children refused cycloplegia at any visit. This may have resulted in a more myopic prescription measured using autorefraction thereby overestimating the amount of myopia they have. However, the use of axial length and vitreous chamber measurements to evaluate myopia progression do not require cycloplegia for an accurate measurement.54 Additionally, axial length measurements are considered the preferred method to assess the progression of myopia considering their usefulness as a diagnostic factor for disease 55 and their high level of precision.54 Therefore, the measurements of axial length and vitreous chamber depth continued to provide an objective and accurate indicator of myopia progression in these children.
The study monitored myopia progression over a 6-month period. As myopia progression can vary seasonally,56 the data does not account for any seasonal variations in myopia. Despite this, research suggests that deviation from normal growth pattern may be identifiable just after a 6-month period using modern biometry methods.57
Conclusions
Light therapy may provide a tolerable and feasible inter-vention for slowing myopia progression. Due to the wide availability of MMI in the UK, future research may wish to consider alternative study designs including the use of virtual controls or a cross over design to mitigate future recruitment challenges. Further research is required to confirm if BLT can slow axial elongation and promote choroidal thickening in a large cohort of myopic children over a longer time period.
Ethical approval and consent to participate
Ethical approval was granted by the Health and Life Sciences Ethics Committee at Glasgow Caledonian University (HLS/LS/A22/074) and the study was conducted in accordance with the declaration of Helsinki. Informed consent was obtained from parents and informed assent obtained from children prior to participation.
Availability of data and materials
The data that support the findings of this study are available from the corresponding author upon reasonable request.
Competing interests
The authors have no competing interests to declare.
Funding
This study was funded by the Carnegie Trust (RIG012527).
Acknowledgements
The authors would like to acknowledge Lumie® for the pro-vision of Vitamin L lamps for the study.
COE Multiple Choice Questionnaire
The publication "The feasibility and tolerability of bright light therapy in childhood myopia: A pilot study" has been approved as a COE continuing education article by the German Quality Association for Optometric Services (GOL). The deadline to answer the questions is 1st October 2026. Only one answer per question is correct. Successful completion requires answering four of the six questions.
You can take the continuing education exam while logged in.
Users who are not yet logged in can register for ocl-online free of charge here.
meta-analysis. Clinics (Sao Paulo).79, 100375.
Interventions in Children. JAMA, 6, e2340986.
affective disorder. J. Am. Acad. Child. Adolesc. Psychiatry, 36, 816-821.