Myopia management in children: the 2024 UK/Ireland expert consensus
Purpose: With rising prevalence, myopia and its management are becoming an increasing important topic in the professional portfolio of optometrists, opticians and ophthalmologists. This article aims to provide a summary of the recent United Kingdom (UK)/Ireland consensus on myopia management in children and adolescents, and to place it in perspective by comparing its recommendations with German, European and International guidelines.
Material and Methods: This narrative review highlights key statements resulting from the consensus, which used online meetings, discussions and surveys to build agreement.
Results: The UK/Ireland consensus offers recommendations for assessment, management and monitoring of myopia in children and young people. Key statements include that children with early-onset high myopia and features suspicious of underlying conditions should be referred to an ophthalmologist for further investigations. Children who may benefit most from myopia management interventions are those with fastest progression, i.e. those under the age of 13 years. Optical interventions, such as peripheral-plus spectacles or contact lenses, are considered first-line treatments, and low-concentration atropine may be an option once available commercially. Lifestyle modifications such as increasing the time spent outdoors are recommended to delay myopia onset and slow progression, though more research is needed on near-work and lighting conditions. The panel also emphasized the importance of equitable access to treatments, especially in light of financial barriers.
Conclusion: As evidence on effectiveness and efficacy of myopia management interventions in European populations is building, recommendations for practice show increasing alignment.
Introduction
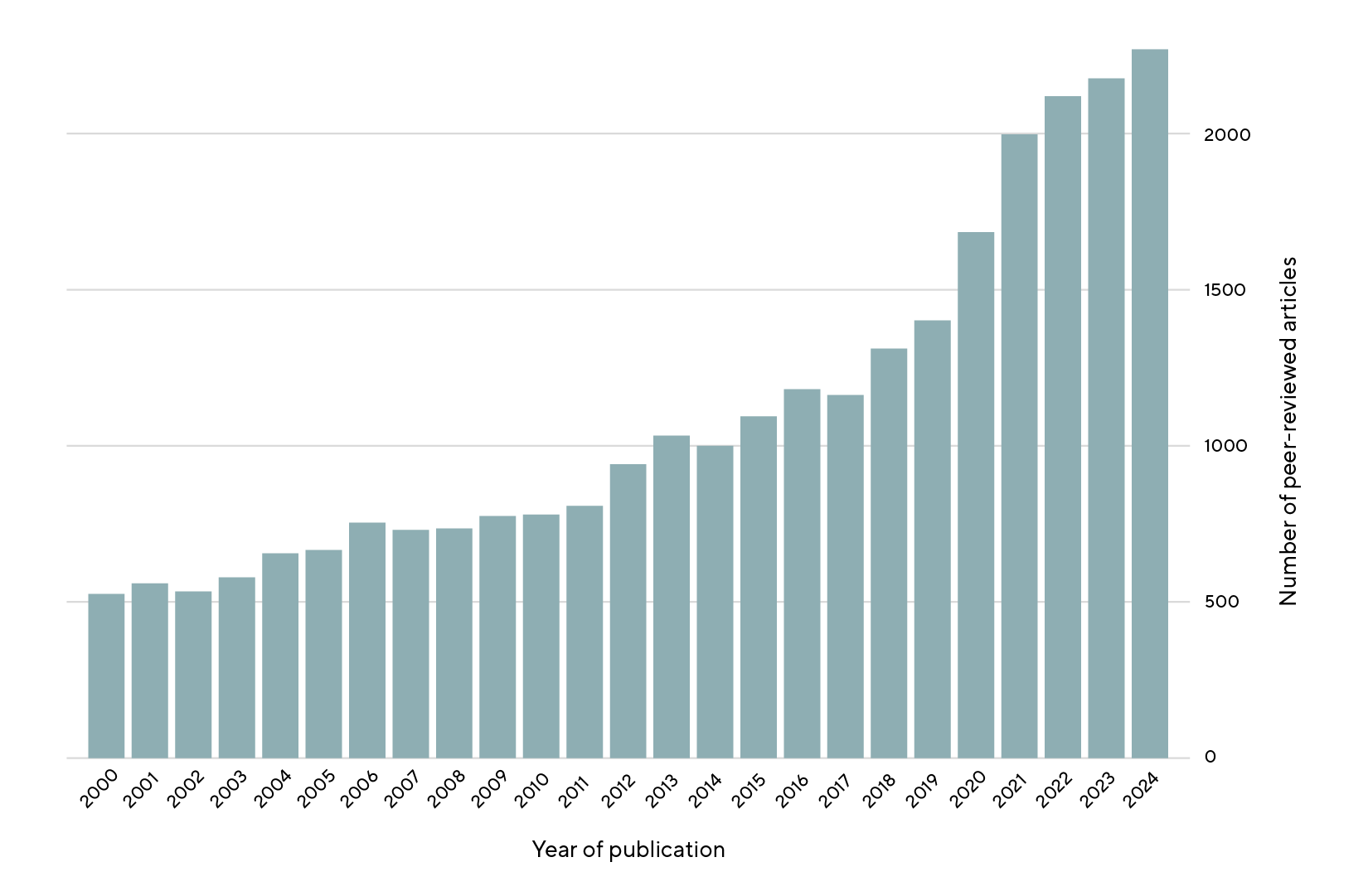
Myopia prevalence is on the rise globally, with significant increases in the number of affected children and young people (CYP) reported in East Asian countries. Trends in Western countries are variable, with prevalence ranging from around 8 % in younger school-aged children in Germany 1,2 to around 29 % in 12-13 year-old children in the UK.3,4,5 Myopia management in children is becoming an increasingly important topic for primary care ophthalmic practitioners, i.e. optometrists, opticians and paediatric ophthalmologists.6 With the growing interest and options available for management, more research than ever before is being conducted into myopia, and it may be hard for busy clinicians to tease apart any nuances and big picture from the published literature. For example, a PubMed search for articles with the key word of myopia indicates the number of articles published per year increased nearly exponentially, from 523 in 2000 to 2262 in
2024 (Figure 1).
In the UK and Ireland, a group of expert researchers and clinicians conducted a Delphi consensus to develop agreement on a wide range of myopia-related questions.7 This aimed to develop recommendations specific for the UK landscape, where primary eye care is provided by optometrists in the community and high street practice,8 including myopia management in children.9 In other European countries, optometrists currently have far less autonomy in prescribing glasses and contact lenses (European Journal of Ophthalmology, EJO, manuscript submitted), but as the workforce develops, myopia management will increasingly enter their practice, and these practitioners should expect more queries from potentially worried parents.
This article aims to provide a summary of the UK/Ireland consensus, and to place it in perspective by comparing its recommendations with German, European and International guidelines.10,11,12,13
Material and Methods
For this narrative review, we summarised salient points from the recent UK/Ireland consensus on myopia management in children. The consensus exercises used a modified Delphi process with the following steps:14,15 a launch meeting to agree the format workflow, scope and topic areas, followed by four anonymous web-based survey rounds using commercial Delphi software, Welphi (welphi.com) to generate (survey round 1), refine (survey round 2), and vote on all items (rounds 3 and 4). A second meeting was held to discuss items that had not reached consensus, and to carry out a final round of voting. The thresholds for agreement were pre-specified.14,15
Results
How should we define myopia?
The UK/Ireland consensus recommends to use the definitions and thresholds proposed by the International Myopia Institute (IMI), of −0.50 D and −6.00 D mean spherical equivalent using cycloplegia for myopia and high myopia, respectively.10
How important is equitable access to new treatments?
In principle, public funding should be made available, supported by further epidemiological research to enhance evidence on prevalence, progression and severity of myopia in European countries. The UK/Ireland panel considered the current published evidence about efficacy/effectiveness to be sufficiently strong to be able to recommend interventions.7
How should children and young people with myopia be assessed, and who should be referred to an ophthalmologist?
The eye care professional should ask about a family history of myopia and high myopia, the child’s history of retinopathy of prematurity (ROP) and other relevant systemic conditions, as well as about other conditions and syndromes. Children and young people with myopia whose best-corrected visual acuity is significantly reduced for their age at more than one visit, and those younger than 10 years with both high myopia and features possibly indicating other underlying conditions should be referred to an ophthalmologist for further
investigation.2
Which lifestyle and behavioural recommendations can we make?
Spending time outdoors may delay the onset of myopia and have a small beneficial impact on myopia progression. The exact duration of time outdoors required is uncertain, but 2 hours/day may have a protective effect. The UK/Ireland panel considered that evidence for specific working distances, for example holding books/screens at 30 cm or beyond from the face, or for “good lighting” at the desk is still insufficient to make recommendations.7
When and how should myopia management/control be started?
The UK/Ireland consensus panel agreed that interventions should be discussed with all families of children at risk of or demonstrating myopia progression, including those with onset of myopia before the age of 5 years. However, more evidence is needed whether these interventions would also be effective in children with underlying eye or syndromic conditions.7
A discussion about myopia-management should be held for children who develop myopia before the age of 13 years, without the prior need to monitor progression. The young person should be involved in the discussion of different management options.7
What is the state of play with optical options?
Myopia-management contact and spectacle lenses can be used as a first-line therapy; no single optical intervention has demonstrated superiority over others.16 Therefore, decisions regarding which treatment is most suitable should include CYP, parent and practitioner, taking into account the child’s lifestyle and preferences. It is considered safe to use optical interventions in the presence of heterophoria, with appropriate monitoring of binocular function. Where astigmatic errors cannot be fully corrected by myopia interventions, but visual acuity is acceptable, the use of these interventions is at the discretion of the eye care professional.7
What is the state of play with pharmaceutical options?
At present, no commercial preparation of low-concentration atropine is available in Europe. Once these do reach the market, they should be considered as a first- or second-line intervention for myopia-management, and could be used in combination with optical approaches. Risks and benefits should be discussed with families to achieve a joint decision about starting atropine. In the UK/Ireland consensus, moderate agreement supported the management approach that children who, based on eye growth charts, have a 95 % risk of developing axial length greater than 26 mm should be offered additional treatment early, if progression does occur.7
How should myopia progression and management be monitored?
Before starting any intervention, non-cycloplegic axial length (AL), cycloplegic (auto)refraction/retinoscopy and near point and/or amplitude of accommodation should be measured, if available. Non-cycloplegic AL measurements should be repeated every 6 months and can be tracked using published eye growth curves. Cycloplegic autorefraction and/or retinoscopy should be performed where AL measurements are not available.7
If visual acuity whilst wearing a myopia-intervention is worse than 0.3 logMAR or more than 1-2 lines worse than best-corrected visual acuity, the practitioner should check adherence and any other contributing factors and consider discontinuing that option. Adverse events of optical/pharmacological interventions should be reported, using national adverse event reporting processes.7
When do we know that the treatment is successful?
Change to a lower percentile on an eye growth chart/nomogram may potentially indicate success in slowing progression. Cycloplegic spherical equivalent progression by −0.25 D/year or less may be an indicator of success. However, the annual rate of progression, both axial elongation and spherical equivalent progression, depends on the child’s age and ethnicity, and using rigid thresholds in practice is not helpful.
If progression control is insufficient at 6 months after the start of treatment, adherence should be discussed. If successful control is not achieved at 12 months despite good adherence, a pharmacological approach should be considered, once market-authorisation for low-concentration atropine is in place.7
What initial and ongoing training should myopia practitioners complete?
Eye care professionals should be offered evidence-based training independent from intervention manufacturers, and those prescribing interventions should undertake appropriate training. Eye care practitioners should collate a yearly audit of progression rates in children under their care.7
When can myopia management be stopped?
Currently it is difficult to know exactly when is best to stop a myopia management intervention. Interventions may need to be continued into early adulthood, with ongoing monitoring until myopia stabilises. Restarting interventions should be considered if there is further progression after prior use. More evidence for „tapering“ regimes for low-concentration atropine, i.e. a gradual reduction in concentration and/or frequency, is needed.7
Discussion
The UK/Ireland 2024 consensus provides detailed and specific recommendations for the management of myopia in children and young people.
Its methodology, using the well-established Delphi consensus method and inclusion of a wide range of expert stakeholders, ensured its internal validity. Overall, recommendations were similar to those made by other national and international bodies, with some exceptions.
The European Society of Ophthalmology (ESO) guidance acknowledges that family finances play a role in the choice of a myopia management intervention (MMI).11,12 Indeed, in some European countries myopia-management glasses may be provided by the public health system, whilst in others, low-concentration atropine produced by a hospital pharmacy may be prescribed free of charge (EJO, manuscript submitted). In the UK, no MMI is publicly funded, whilst standard single-vision glasses are funded by the National Health Service for children and young people up to the 16th birthday (or 18th if they remain in full time education). Families often find it difficult to afford MMI, and the UK/Ireland panel endorsed public funding on the grounds of strong evidence for good efficacy/effectiveness of selected interventions. Decisions about public financing of MMI in Europe are hampered by the lack of data on a potential reduction in long-term health and social care costs for late complications associated with myopia. Relevant studies are underway.
Like ESO and IMI guidance, the UK/Ireland consensus recognises that early-onset high myopia may indicate underlying pathologies, such as retinal dystrophies, connective tissue disorders and other syndromes,10,11,12 and that affected children should be referred to an ophthalmologist for further investigations. The recent IMI publication on management of high myopia provides useful guidance,17 which was reflected in the UK/Ireland consensus: reduced best-corrected visual acuity and features associated with underlying conditions warrant referral.
As for myopia assessment and monitoring, axial length measurement is recognised as the most accurate measure and is widely recommended, but as it is recognised that at present, only few optometry practices have access to a biometer, cycloplegic spherical equivalent is often accepted as alternative.10,7,11,12
Spending time outdoors, around 2 hours a day, or 8-15 hours per week, is recommended by all guideline panels.10,7,11,12,13 However, as data on the role of near-focus work and desk lighting are currently limited, the UK/Ireland panel felt that recommendations on near work and desk lighting could not yet be supported.7 European Society of Ophthalmology, IMI and German guidelines, however, incorporate relevant recommendations about near-work and indoor
lighting.10,11,12,13
When to start myopia management interventions is still a topic of debate. Whilst the definition of myopia usually follows the IMI definition of −0.50 D, the age of the child/young person also needs to be taken into consideration. Progression is fastest until the age of around 12 years, and the UK/Ireland panel therefore recommended MMI for young people presenting with myopia before the age of 13 years.7 In older children, the effect of interventions will be less than in younger children, but many will still wish to use them, to achieve a reduction in final degree of myopia in adulthood. Other guidelines do not include an age criterium for starting treatment.10,11,12,13 All guidelines agree that the choice of intervention should take into account the child’s and family’s lifestyle;10,7,11,12,13 the UK/Ireland consensus adds that the child should be involved in the discussion, and that their opinion must be respected.7
There is no evidence at present that one type of intervention is superior to others,10,7,11,12,13 and guidelines tend to recommend myopia-management spectacles, contact lenses, or low-concentration atropine as evidence-based first-line treatments.10,7,11,12,13 The UK/Ireland consensus panel was cautious with regards to low-concentration atropine, reflecting the lack of availability of this option in practice, and the conflicting evidence about efficacy of 0.01 % and 0.02 % atropine in Western populations.7 Overall, clinical trials suggest that low-concentration may be effective, but the optimal dosage is still unclear. Younger children, in whom progression is faster, may have a greater benefit from 0.05 % than 0.01 %,12,18 but commercial preparations of low-concentration atropine are not yet available in Europe. Whilst commercial preparations prepared to strict quality management standards carry significant advantages, such as assurance about shelf-life and reduced risk of contamination,14,15 some European hospital still use locally compounded preparations; the German guidelines include the formula for producing low-concentration atropine.13
Agreement is building that myopia management interventions should be continued until myopia has stabilised; the exact timepoint has not yet found consensus. The European guidelines state that in 95 % of people, myopia stabilises by the age of 24 years, and that a useful criterium for stabilisation is axial length progression of 0.06 mm or less per year.12 Axial elongation nomograms displaying meta-analysis data from population-based studies and the control groups form clinical trials are useful to assess ongoing treatment effect.19,20
Differences in availability and price of MMIs and differences in workforce between countries limit the generalisability of the UK/Ireland consensus. Whilst in the UK, optometrists are the principal providers of eye care for children with myopia, in other countries this role falls to ophthalmologists, and occasionally orthoptists (EJO, manuscript submitted).
Conclusions
As evidence on effectiveness and efficacy of MMI in European populations is building, recommendations for practice in different nations show increasing alignment. Incorporating recent publications in the field, the 2024 UK/Ireland consensus provides specific considerations useful for practice.
Acknowledgements
A. Dahlmann-Noor is supported by the NIHR Moorfields Biomedical Research Centre. The views expressed in this paper are not necessarily those of the individual authors, the NHS, the NIHR, or the Department of Health. The authors would also like to acknowledge all of the participants and co-authors that took part in the UK and Ireland Myopia Delphi Panel study.
COE-Fortbildungsprüfung
Die Publikation „Myopie-Management bei Kindern: Delphi-Konsensbericht 2024 für Großbritannien und Irland “ wurde von der Gütegemeinschaft Optometrische Leistungen (GOL) als COE Fortbildungsartikel anerkannt. Die Frist zur Beantwortung der Fragen endet am 1. Juni 2026 Pro Frage ist nur eine Antwort richtig. Eine erfolgreiche Teilnahme setzt die Beantwortung von vier der sechs Fragen voraus.
Die Fortbildungsprüfung können Sie im eingeloggten Zustand absolvieren.
Noch nicht angemeldete Nutzer*innen können sich hier kostenlos für ocl-online registrieren.
(2010). Ethnic Differences in the Prevalence of Myopia and Ocular Biometry in 10- and 11-Year-Old Children: The Child Heart and Health Study in England (CHASE). Invest. Ophthalmol. Vis. Sci., 51, 6270.
Practice-2022 Update. Invest. Ophthalmol. Vis. Sci., 64, 12.
Allen, P. M., Beach, M. L., Bruce, G., Buckhurst, H. D., Buckhurst, P. J., Cruickshank, F. E., Cufflin, M. P., Day, M. D., Doyle, L., Evans, B. J. W., Flitcroft, D. I., Gray, L. S., Grewal, I., Guggenheim, J. A., Hammond, C. J., Higginbotham, J. C., Jawaid, I., Kearney, S., Lawrenson, J. G., Logan, N. S.,
Loughman, J., Mallen, E. A. H., McCullough, S. J., Nagra, M., Saunders, K. J.,
Seidel, D., Shah, T., Strang, N. C., Webber, K. J., Wolffsohn, J. S., Young, A. L.
(“024). 2024 UK and Ireland modified Delphi consensus on myopia management in children and young people. Ophthalmic Physiol. Opt., 44. 1368-1391.
A workforce modelling study. Ophthalmic Physiol. Opt., 42, 1092–1102.
Nagy, Z. Z. Kestelyn, P. G., Januleviciene, I., Grzybowski, A., Vidinova, C. N.,
Guggenheim, J. A., Polling, J. R., Wolffsohn, J. S., Tideman, J. W. L., Allen, P. M.,
Baraas, R. C., Saunders, K. J., McCullough, S. J., Gray, L. S., Wahl, S., Smirnova, I. Y., Formenti, M., Radhakrishnan, H., Resnikoff, S., Németh, J.; SOE Myopia Consensus Group. (2023). Myopia management algorithm. Annexe to the article titled Update and guidance on management of myopia. European Society of Ophthalmology in cooperation with International Myopia Institute. Eur. J. Ophthalmol., 34, 952-966.
Moore, A. T., Nischal, K. K., Ohno-Matsui, K., Paysse, E. A., Repka, M. X.,
Smirnova, I. Y., Snead, M., Verhoeven, V. J. M., Verkicharla, P. K. (2023). IMI-Management and Investigation of High Myopia in Infants and Young Children. Invest. Ophthalmol. Vis. Sci., 64, 3.
