Perforating corneal injury, scleral rupture and mini-scleral contact lenses
Purpose: This case report describes the contact lens rehabilitation of a patient using a mini-scleral contact lens following a perforating corneal injury and scleral rupture.
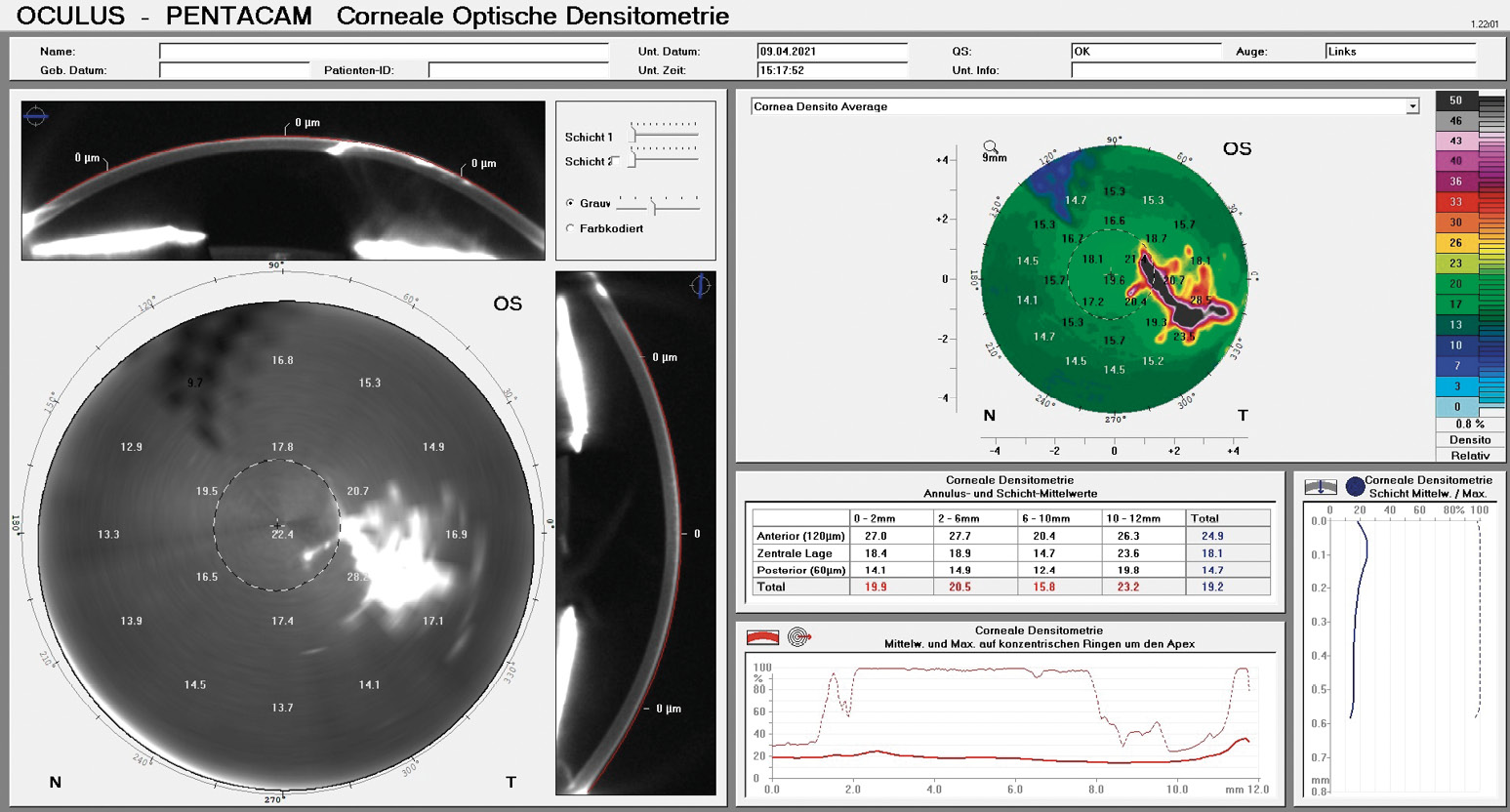
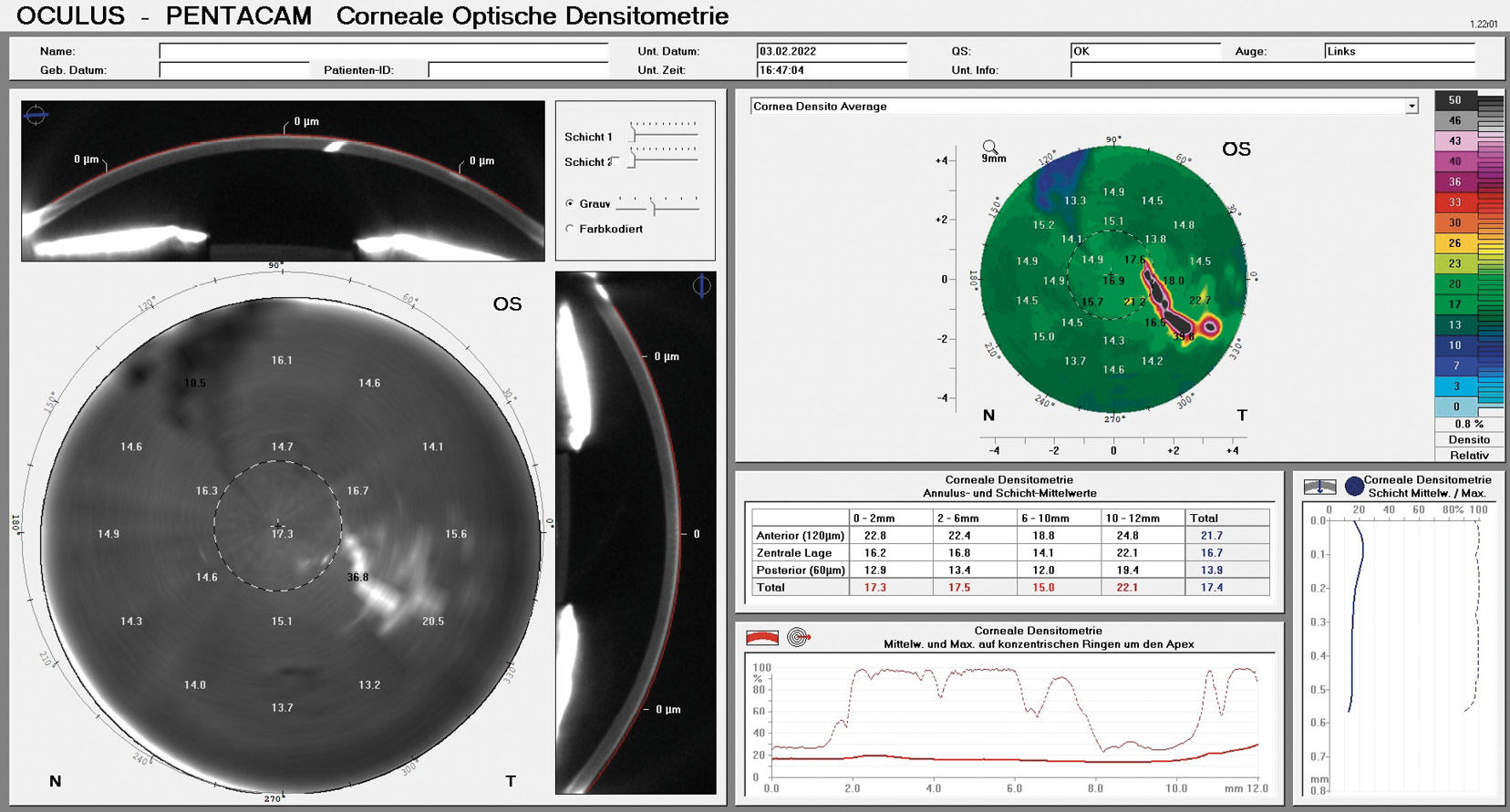
Material and Methods: Based on detailed anterior segment tomography of the affected eye, the complete fitting process of a mini-scleral contact lens is described with the aim of achieving the best possible visual rehabilitation of the injured eye. This includes the determination of the contact lens parameters through the interpretation of the best possible fluorescein image as well as the visualisation of the corneal injury using the densitometry program of the Oculus Pentacam.
Results: With the help of the fitted mini-scleral contact lens, full visual rehabilitation of the injured eye was achieved. The last follow-up appointment after 8 months showed an excellent subjective and objective tolerance of the contact lens. Furthermore, a clear healing process of the corneal injury was observed.
Conclusions: The visual rehabilitation of corneal injuries as well as corneal ectasia of various types has always been one of the classic indications for RGP contact lenses. For complex corneal shapes, fitting mini-scleral contact lenses should also be considered.
Introduction
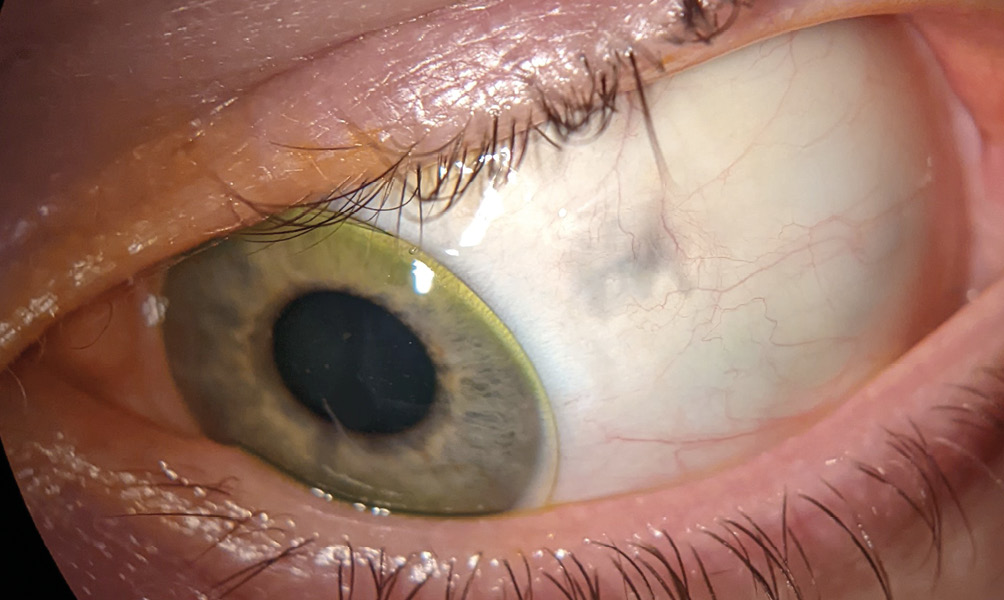
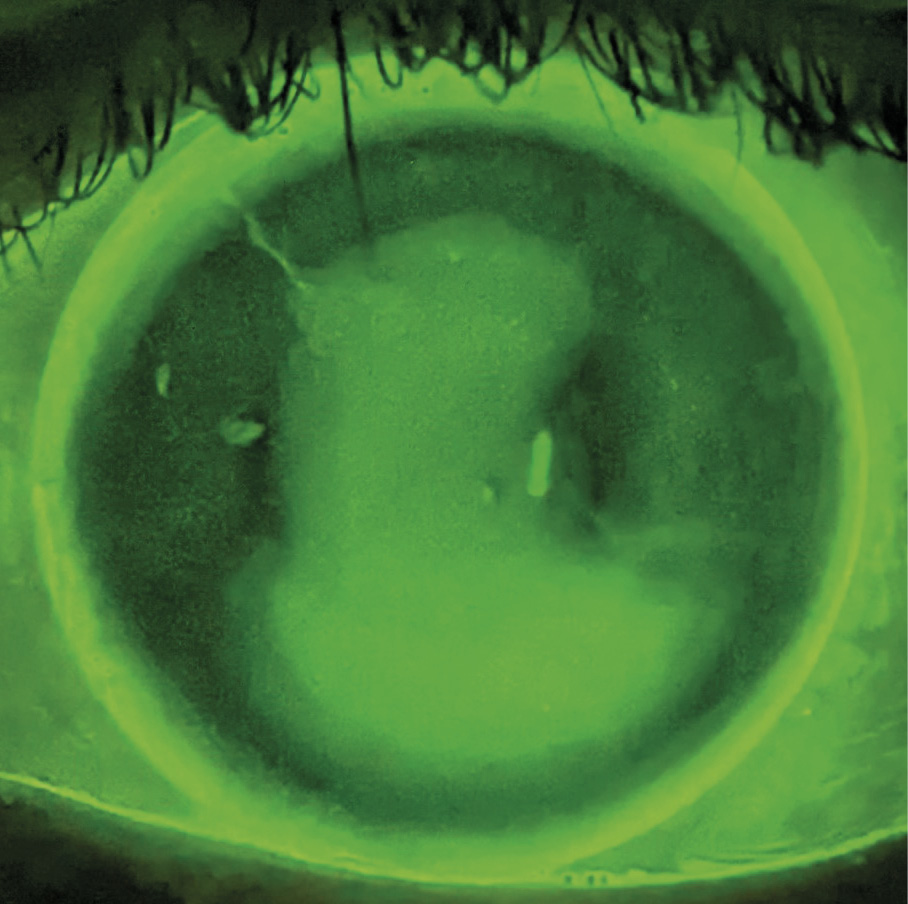
A 26-year-old female patient visited our eye and vision center for RGP contact lens fitting for her left eye. This visit was preceded by an accident on a private construction site, in which a cable had detached, and the socket located at its end hit the patient in the face. The left spectacle lens shattered in the process. The report issued by the eye clinic visited right after the accident mentions that the slit lamp exam showed a perforating corneal injury and a scleral rupture (Figure 1). A CT scan of the skull and orbit showed no intraocular foreign body. Antibiotic and anti-inflammatory therapy was initiated after the emergency suture of the cornea and sclera and the patient was hospitalised for 7 days in the clinic. The final report of the eye clinic for the left eye was as follows:

Distant visual acuity: 0.1 sc, with stenopaeic slit = 0.32, IOP by palpation: normal
Anterior eye segment:
- Conjunctiva: tight sutures, injected
- cornea: Soft therapeutic contact lens in loco, tight sutures, wound adapted
- Anterior chamber: deep, pupil round and reactive to light, crystalline lens clear
Fundus:
Optic nerve head without abnormality, normal macula according to age, retinal attachment as far as can be assessed
Material and Methods
The first examinations were carried out in our eye and vision centre 10 weeks after the hospital discharge, the stitch removal and the release for contact lens fitting by the clinic. The right eye showed no irritation on the eyelids and conjunctiva. The cornea was clear, the anterior chamber was optically empty and deep, the pupil was round and reactive to light. The crystalline lens was clear. The tear meniscus was > 0.2 mm and the tear film normal. The left eye also showed no irritation on the eyelids and conjunctiva. The corneal scar and the well healed scleral rupture were clearly visible during the slit lamp exam (Figure 2 and Figure 6).
The tear meniscus was > 0.2 mm, similar to the right eye, and the tear film normal. The corneal diameter was 12.1 mm.
Visual acuity, refraction and corneal topography of the left eye were as follows:
Visual acuity
Visual acuity O.D.: 0.32 sc 1.0 cc
Visual acuity O.S.: 0.16 sc 0.4+ cc
Refraction
O.D.: -1.0 D cyl -0.25 D axis 131°
O.S.: +2.5 D cyl -8.0 D axis 174°
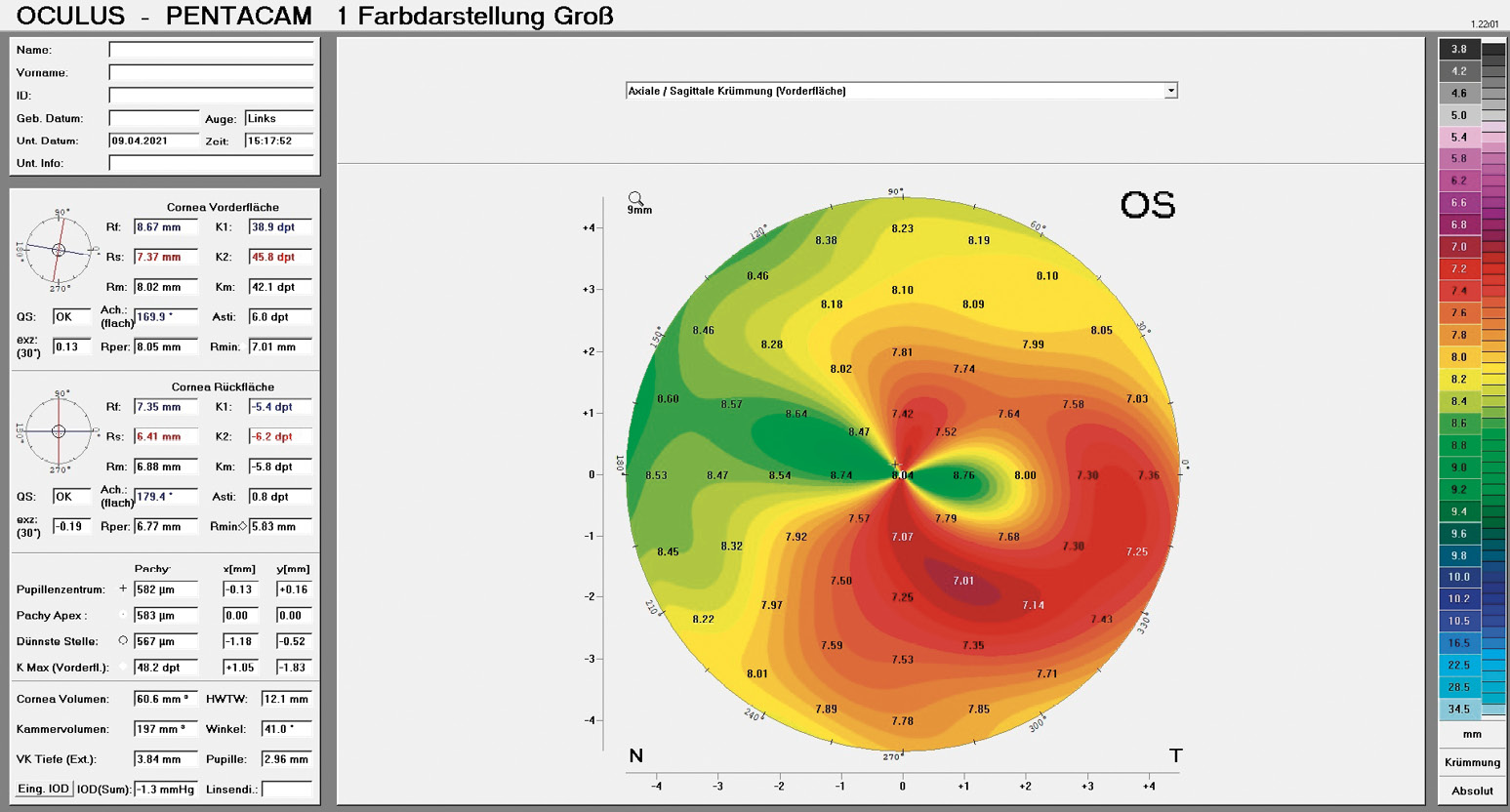
Corneal topography OS
The central corneal radii were 8.67 mm at 170° and 7.37 mm at 80° with an average eccentricity of 0.13 (Figure 3).
Determining the lens parameters
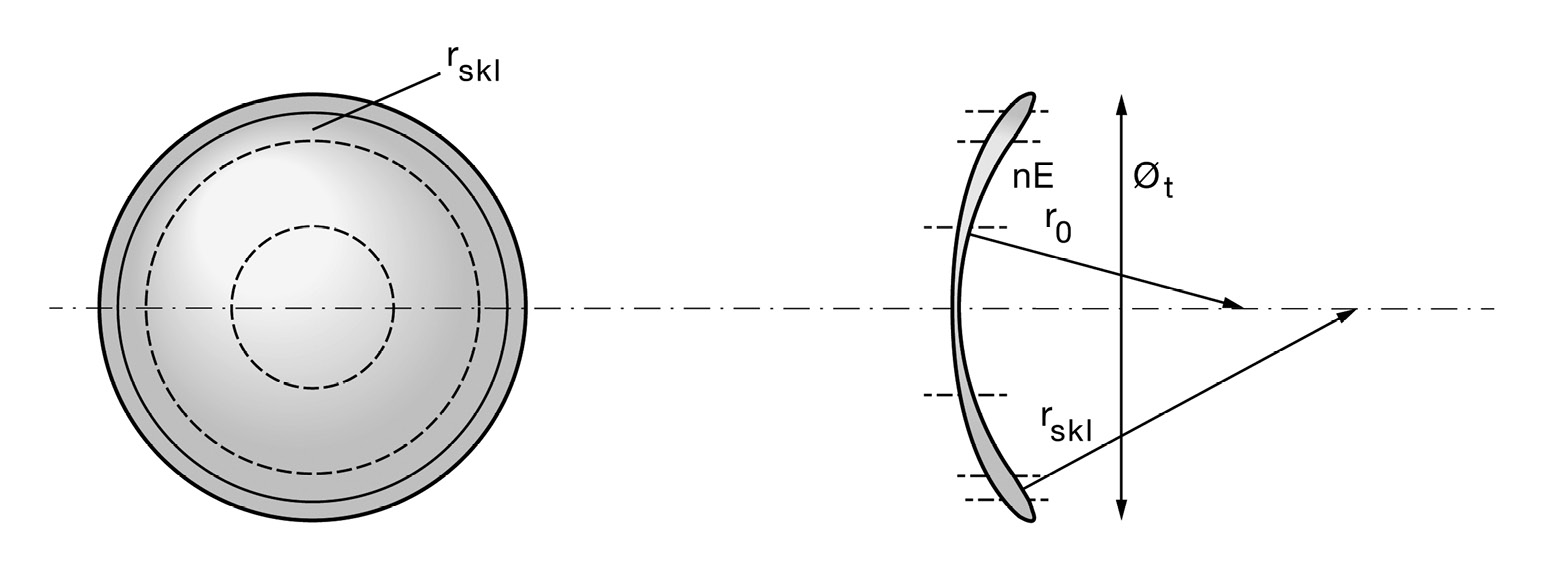
Based on the refraction, the corneal and scleral findings as well as the topography, we decided to fit a rotationally symmetric, aspheric, small mini-scleral contact lens from Falco, Switzerland. The scleral zone radius and the diameter of the scleral zone can be individually selected for this type of lens, along with other lens parameters (Figure 4). The parameters of the first lens prescribed were as follows:
Diagnostic lens
Lens type: Falco SKA
Central radius: 7.95 mm
Numerical eccentricity: 0.5 Overall diameter: 13.50 mm
Refractive power: -0.87 D
Scleral zone radius: 10.00 mm Diameter of the scleral zone: 10.5 mm
Material: Optimum - Extreme white
Since the visual acuity with this lens was 0.8, but the fit was too flat in the centre and the power of the lens was slightly too high, the prescription lens was modified as follows:
Prescription lens
Lens type: Falco SKA
Central radius: 7.85 mm
Numerical eccentricity: 0.5 Overall diameter: 13.50 mm
Refractive power: -0.75 D
Scleral zone radius: 9.9 mm Diameter of the scleral zone: 10.5 mm
Material: Optimum - Extreme white
Over-refraction: sph. +0.25 D cyl -1.0 D axis 85°
The fit of this contact lens was spontaneously satisfactory both subjectively and objectively - the distance of the lens edge from the well-healed scleral injury, which is important, was given (Figure 5 and Figure 6). The visual acuity was 1.0 with over-refraction, so we decided to use this lens without further modification. Since the patient also needed visual correction due to her visual defect on the right eye, we decided to correct the residual astigmatism with spectacles to achieve a better stability of the visual acuity.
Contact lens hygiene
“Rubicon Clears” and “Rubicon Clear Sol” as well as the wetting agent “drop & see” from Contopharma as a contact lens care system was recommended.
Check-up: (10 months after contact lens prescription)
O.D.: 1.0 (correction: -1.0 D cyl -0.25 D axis 131°)
O.S.: 1.0 (with contact lens and spectacle correction +0.25 D cyl -1.0 D axis 85°)
Binocular: orthophoria; positive stereopsis
The patient was completely satisfied with the visual rehabilitation by the contact lens. The visual acuity was satisfactory, and the contact lens was well tolerated throughout the entire day. The anterior segment of the eye was without findings. The marked regression of the corneal scar compared to the findings 10 months before was striking. This was clearly recognisable with the aid of the densitometry program of the Oculus Pentacam (Figure 7).
Discussion
A perforating eye injury, and here especially a perforation of the cornea, is a serious injury with possible serious complications.1,2 Such an eye injury should always be considered an emergency and requires a fast referral to an ophthalmologist or an eye clinic. Perforating eye injuries can have different causes. The severity depends on the type of injury. This also determines the success of visual rehabilitation using contact lenses.3,4,5 In 2020, Aldahash et al. investigated the epidemiology and aetiology of perforating trauma to the eye in 213 children under the age of 18. The most common type of injury was a puncture injury caused by a knife followed by injuries with metallic objects as well as glass and pencil injuries. The later visual result was directly related to the initial presentation of the injury. In this regard, a retinal injury was a significant prognostic factor of a later deterioration in visual acuity.6 In this context, the now 25-year-old Birmingham Eye Trauma Terminology (BETT) offers a consistent, simple and comprehensive system for describing any type of mechanical eyeball trauma.7 The wound healing in the case of perforating corneal injuries depends on the individual wound healing type. In a recent study, Zheng et al. investigated how long it took for the wound to heal after a perforated corneal injury using OCT technology. The different wound types were classified as follows: type 1: continuous inner wound edge or step height ≦ 80 μm; type 2: step height > 80 μm; type 3: gap between wound edges; and type 4: intraocular tissue adhering to wound. They also compared the surgical results of the different wound types. The majority of wound margins appose between 3 and 6 months after the injury. However, the initial configuration of the wound affected the healing pattern.8,9
Fitting of RGP contact lenses with an irregular cornea as a result of corneal injuries is one of the classic indications of contact lens use.10,11,12 Corneal lenses, mini-scleral lenses, scleral lenses and hybrid lenses are among the possible options.13,14,15,16,17 The terms corneo-scleral, semi-scleral, mini-scleral and scleral lenses have not yet been standardised. In principle, scleral lenses are those with a diameter between 15 mm and 24 mm and that are positioned on the sclera. In contrast, in the case of corneo-scleral lenses or small mini-scleral lenses, the contact zones extend over the peripheral cornea and anterior sclera.18,19 It is precisely the size of the contact lens and the peripheral contact zone which are particularly important in the case of a perforating corneal injury in conjunction with a scleral rupture, in order not to generate any pressure in the wound area. An outstanding issue in the context of the fitting of these lenses is the real horizontal visible iris diameter. Based on extensive literature research, Bergmanson comes to the conclusion that the width of the limbus has neither been structurally defined nor precisely quantified to date, and therefore concludes that new protocols should be developed to determine the dimensions of the average cornea and the limbus.20 The determination of the back surface design of mini- or corneo-scleral lenses can be carried out in various ways. Until recently, this included only an empirical fitting by means of diagnostic lenses based on the measurement results of traditional keratometers or topography systems as well as the interpretation of the fluorescein images. Both methods do not allow for a precise specification of the corneo-scleral profile. In more recent publications, Gier et al., Ritzman et al. and Bandlitz et al. describe automated methods with the aid of which solid data can be obtained for the fitting of such contact lenses.21,22,23 Based on this, the back surface design of (mini-) scleral lenses can be determined not only more individually, but also sometimes more simply.24 This helps significantly and saves time, especially in the case of less experienced practitioners.
Conclusions
The contact lens treatment of different corneal injuries as well as corneal ectasia is in most cases the basis for the visual rehabilitation of the affected patients. Particularly with the resulting more complex contact lens fittings, mini-scleral or scleral lenses are often the treatment method of choice. Due to the larger diameter of these contact lenses, quantification of the corneo-scleral profile (CSP) is of great benefit for their fitting.
Conflict of interest
The author has no conflict of interest with respect to the methods, devices and products referred to in the article.
