Unilateral lens coloboma causes anisometropia
Purpose: This case report describes the surgical treatment of a unilateral coloboma of the crystalline lens in a 55-year-old female patient.
Material and Methods: Underdevelopment of the crystalline lens on the left eye resulted in severe lenticular astigmatism with a significant anisometropia with extreme high order aberration. The degree of anisometropia was too high for glasses to be worn comfortably. To reduce the anisometropia and to increase binocular vision quality, a lensectomy was performed with implantation of an Artisan Aphakia 205 (Ophtec BV, Netherlands) intraocular lens.
Results: The postoperative refractive error on the left eye was sph. +0.25 cyl. −0.75 axis 83° and the visual acuity was 20/20. As refractive error and visual acuity were nearly the same in both eyes, the patient only occasionally needed reading glasses.
Conclusion: In most cases, severe lens astigmatism with significant anisometropia and extremely high aberration cannot be satisfactorily corrected with glasses or contact lenses. However, this case report shows that it is possible.
Introduction
A 55-year-old female patient visited our local ophthalmology and optometry clinic for a routine eye examination. The patient complained of poorer vision in his left than in his right eye. The detailed medical history of previous ocular traumata and injuries was negative. No previous eye surgery or infections were reported. It could not be determined with certainty whether glasses were worn by the patient as a young child. Except for reading glasses, the patient was not currently wearing any glasses or contact lenses. As an adult, the patient had once tried wearing glasses, but found them uncomfortable and subjectively felt that they did not provide any visual improvement. The patient's general medical history was unremarkable. He was not currently taking any medication. There were no known systemic diseases.
The patient has given written consent for the use of her data in anonymised form.
Material and Methods
Diagnostic Evaluation
Slit lamp examination of the anterior segment of both eyes showed no abnormalities. The intraocular pressure was 12 mmHg on the right eyes and 16 mmHg on the left eye.
Subjective refraction, uncorrected vision and visual acuity was:
O.D.: sph. +1.00 −0.50 axis 20°; uncorrected vision: 20/20; corrected visual acuity: 20/20
O.S.: sph. −1.00 −9.00 axis 95°; uncorrected vision: 20/400; corrected visual acuity: 20/60
Undilated examination of the posterior segment of both eyes showed a clinically healthy retina, with a dry macula, normally structured blood vessels, and unremarkable retinal periphery without degenerative areas.
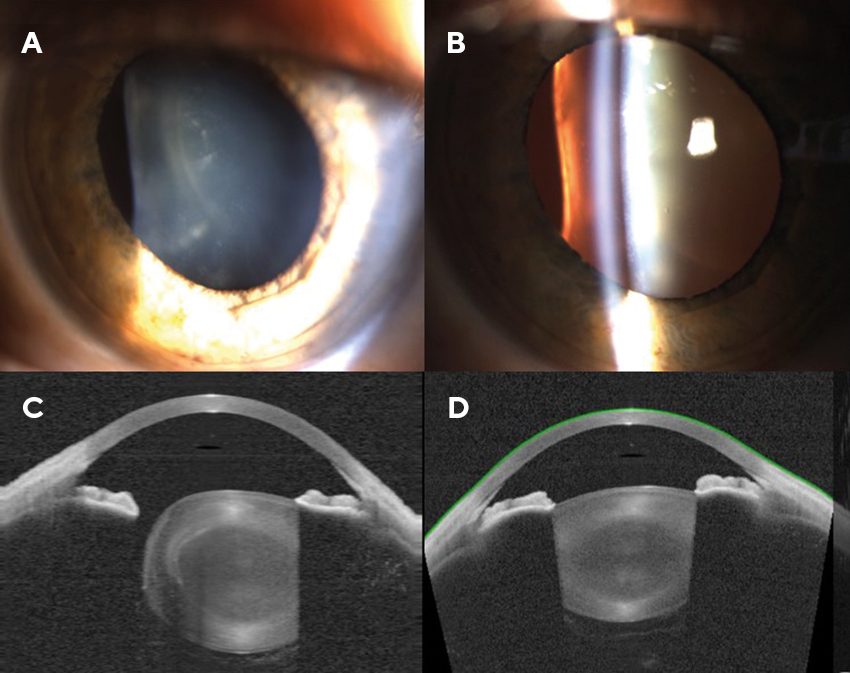
Dilated examination showed a lens coloboma in the left eye. There were no clinical signs of previous trauma in either eye.
Figure 1 shows the lens of the left eye. The right eye is also shown for comparison.
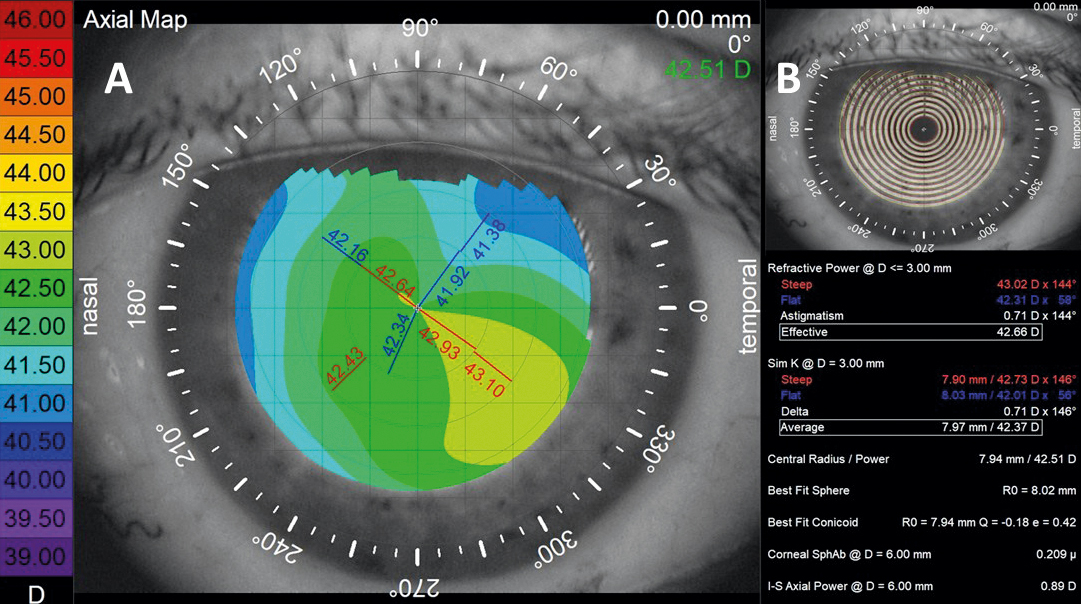
Corneal topography (Figure 2) showed a corneal astigmatism (−0.71 D 60°), which was less than the refractive astigmatism of −9.00 D.
Treatment Strategy
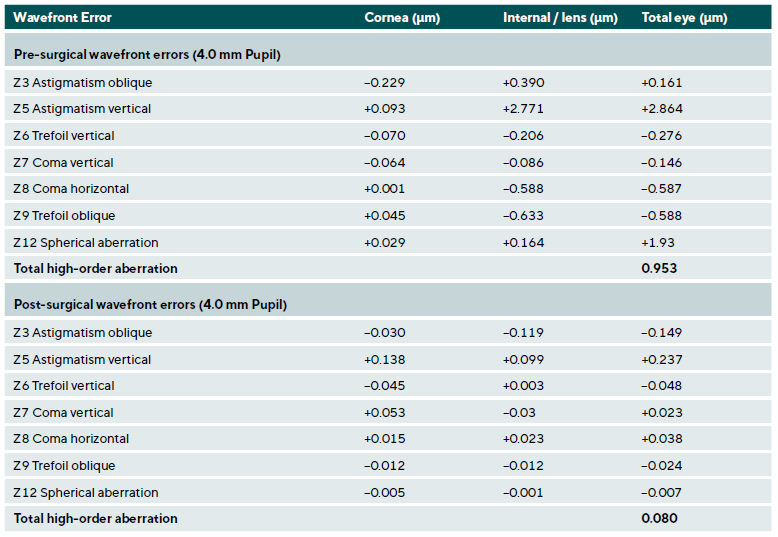
Cause of high astigmatism was the underdeveloped shape of the eye lens (Table 1). For that reason a lensectomy with implantation of an Artisan Aphakia 205 (Ophtec BV, Netherlands) intraocular lens (IOL) with a power of +16.50 D, corresponding to a spherical equivalent refraction (SEQ) between 0.55 and −0.17 D was performed. The therapeutic treatment was a lensectomy combined with a pars plana vitrectomy. With lensectomy, the entire supporting apparatus of the lens was removed (zonular fibres and capsular bag) and the Artisan IOL was implanted retroiridally on the iris. The surgery was performed under general anesthesia.
Postoperative Outcome
The postoperative refractive result was sph. +0.25 @ cyl. −0.75 axis 83°; visual acuity was unexpectedly good at 20/20. Based on the known refractive data, a clear reduction in the cylinder was expected, resulting in a decrease in anisometropia. However, amblyopia of the left eye was also to be expected. For that reason the patient was informed in detail before the surgery about the expected reduced visual acuity of the left eye. However, to the surprised of both the patient and the treatment team, this did not happen.
Discussion
A coloboma is a maldevelopment of the lens that occurs between embryonic day 22 and week 5.1 It can affect any structure in the eye, as it is an embryonic defect. The location and tissue in which the coloboma occurs determine its effects on vision and the development of visual acuity.
Ida Mann published 1937 that a lens coloboma is probably not a coloboma in the classical sense.2 In her opinion, a lens coloboma occurs secondary to a deficiency of zonular fibers. Due to the local absence of zonular fibres, there is insufficient tensile force on the tissue in a localized part of the developing lens. This causes a notch to develop in this area of the lens. The subsequent lens tissue can either thicken or thin locally due to the lack of force, and the shape becomes irregular.3
Glasses and contact lenses are commonly prescribed for astigmatic correction. However, a soft toric contact lens with high astigmatism correction can cause visual disturbances due to their rotation when blinking. The regular topography (Figure 2) was the reason why the refractive error was not corrected with an RGP contact lens. This means that contact lenses no longer have the effect of reducing aberrations, as they do in cases such as keratoconus.
In the present case, a refractive laser treatment for the cornea was possible.4 Corneal thickness was sufficient and the topography was regular. However, it should be noted that in this case, immense astigmatism would have to be ablated in a nearly spherical cornea to achieve a good refractive result. The induced astigmatism will interfere with the development of a cataract later in life. In cataract surgery, the induced corneal astigmatism would have to be neutralized with a toric intraocular lens. However, since correcting the astigmatic refractive error alone, as with glasses, would not result in a significant improvement in visual acuity due to the presence of higher-order aberrations, both options were ruled out.
By removing the crystalline lens in the lensectomy, a drastic reduction in the total aberration of the eye (from 0.953 µm to 0.080 µm) compared with that in a normal population was observed.6 Thus, the best-corrected acuity before surgery was limited not because of the high refractive astigmatism but of the existing immense high-order aberration (HOA). The preoperative examination revealed a lack of zonular fibre that increases the complexity of the surgery.7,8 Therefore, the decision not to perform lens replacement with implantation of a standard IOL into the capsular bag was made due to the high risk of surgical failure. It is certainly be possible to perform an eccentric capsulotomy and implant the IOL together with a capsular tension ring into the capsular bag.9 However, in cases of capsular bag instability, an IOL tilt may occur and lead to unpredictable HOA. For reasons of better and more predictable placement of the IOL, the implantation of an iris-fixed IOL was decided. Postoperatively, the HOA value was lower and corresponded to the normal HOA value of the human eye (Table 1).6 HOA estimates of the eye, especially differences between corneal and internal HOA 10, were extremely helpful in our decision making.
One factor that had to be considered in this case was the young age of the patient, as lensectomy causes a loss of accommodation ability. In our case, presbyopia was already present and the patient needed reading glasses to view close objects. Therefore, this disadvantage did not play a significant role in the decision to perform surgery. Performing surgery at a young age has been shown to increase the risk of retinal detachment within the first year after surgery 11, this risk is particularly high in young men.12
The incidence of retinal detachment 13, whether in the early or late postoperative period, is fortunately low 14, with an estimated rate of approximately 0.99 % 12, most frequently occurring within the first year following surgery. Consequently, lensectomy or cataract extraction at a young age should be reserved for cases with a clear and compelling clinical indication because the risk of a retinal detachments post operative is about 4 times increased in comparison to the non-operated population.13 For these reasons, cataract surgery for refractive purposes only is also not recommended.
In the present case, no clinical cataract was observed in the left eye, and the lens transparency was comparable to that of the right eye. However, the lens exhibited significant optical aberrations, resulting in decreased visual function. The patient was informed in detail before the surgery that the expected postoperative visual acuity would probably be worse than that of the right eye. Therefore, the presence of amblyopia was considered very likely. The patient could not provide reliable information regarding her early visual history, particularly with respect to the use of corrective lenses during the critical period of visual development and ocular dominance establishment.15
A detailed discussion with the patient about the possible risks and benefits of the surgery was also held preoperatively. This included information about the warning signs and symptoms associated with retinal detachment and the need for a regular dilated fundus examination.
After this the surgery was determined to be appropriate and subsequently performed.
The visual acuity after surgery was unexpectedly good for both the patient and the surgeon. Contrary to initial expectations and clinical considerations, no signs of amblyopia were detected. However, visual acuity was determined only on the basis of standardized vision tests. No specific attention was given to crowding phenomena, nor were additional tests performed to detect minor signs of amblyopia. One possible explanation for the achievement of full corrected visual acuity (20/20) is, that the lenticular aberrations developed relatively late in childhood, thereby allowing for a sufficiently long period of balanced binocular vision during the critical phase of visual development. However, this hypothesis re-mains unsubstantiated and should be considered highly speculative.
Conclusion
Unilateral coloboma of the crystalline lens is a relative rare condition. In the present case this caused high refractive astigmatism and anisometropia, which could not treated with glasses or contact lenses. The lensectomy with implantation of an Artisan Aphakia 205 (Ophtec BV, Netherlands) intraocular lens (IOL) resulted in approximately the same refractive error and visual acuity in both eyes, why the patient only occasionally needed reading glasses.
Acknowledgements:
Both authors were affiliated with Pallas Klinik AG in Aarau at the time of the patient's treatment. We would like to express our sincere thanks to the dedicated surgical team, whose professional support contributed significantly to the success of the treatment. We would also like to thank the patient for consenting to the publication of her data.
Conflict of Interests:
The authors declare that there is no conflict of interests re-garding the methods and devices mentioned in the article.
Cataract Surgery: IRIS® Registry (Intelligent Research in Sight) Analysis. Ophthalmol. Sci., 3, 100314.